Every day, she donned a mask and was vigilant about washing her hands or using hand sanitizer which made the ensuing fever, headaches, sore throat and COVID-19 diagnosis startling.
Anna (a pseudonym for privacy protection) has been living with HIV for more than a decade. She painstakingly maintains good hygiene knowing firsthand that people with HIV have impaired immune responses, making it more challenging to fight viral infections such as influenza or perhaps COVID-19. HIV may result in increased susceptibility to secondary illnesses such as pneumonia, heart and lung diseases and death.
“I took all the precautions to protect myself, so I never thought I would get it,” said Anna.
An essential worker, Anna continued to work, mask on, during the pandemic. One day, she noticed additional signage on her floor asking people to wear masks and wash their hands regularly. She asked her manager if she should be concerned.
Everything is okay, replied her manager, who further explained that the signage was following county protocols to ensure people were complying with preventative measures.
“The next week I began to feel sick,” said Anna, who is unsure where she contracted SARS-CoV-2, the virus that causes the novel coronavirus. “At first, I thought it was something transient.”
Anna is not alone in her COVID-19 diagnosis.
As of August 19, 2020, the Centers for Disease Control and Prevention (CDC) reported more than 5.4 million cases of COVID-19 and 171,000 deaths in the United States.
Unanswered questions
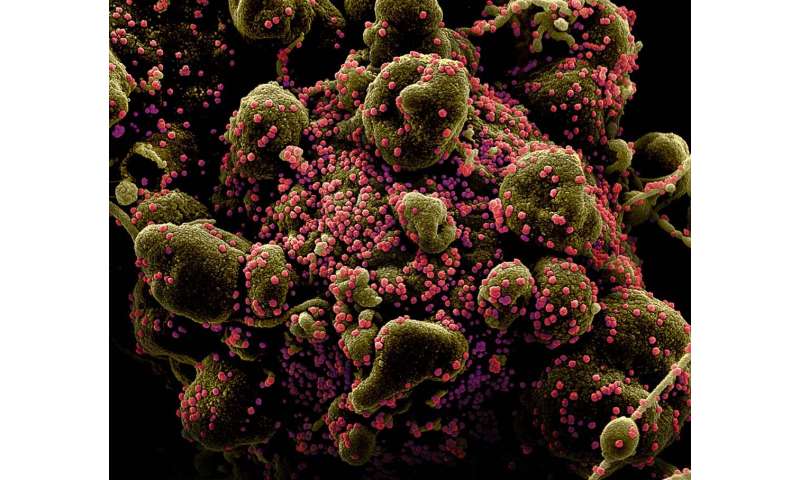
COVID-19 began to make headlines in China in December 2019. Since then, the pandemic has affected millions of lives globally. Scientists rushed to understand the biology and epidemiology of the virus, yet there are still many unknowns.
For example, is SARS-CoV-2 affecting sub-populations of patients with chronic diseases or illnesses differently?
Dr. Edward R. Cachay, an infectious disease physician who specializes in caring for people with HIV, and the team at the Owen Clinic at UC San Diego Health have specific questions about the impact of COVID-19 on their patients.
Are people living with HIV at higher risk for COVID-19 complications? What if the person has the HIV infection under control, will the symptoms be less severe? Are people with HIV more or less likely to contract COVID-19? Will the antiviral medications these patients take help or hinder a SARS-CoV-2 infection?
“These are important questions for this community and their care,” said Cachay. “Many of our friends, brothers, sisters and neighbors are living with HIV. Some of them are living with HIV for a long time and are doing quite well. When another wave of COVID-19 comes, which unavoidably will happen, we want to be more prepared to inform our community, stakeholders and policymakers.”
In an attempt to address some of these questions, Cachay designed a study that looks at what independent predictors, biological or psychosocial, contribute to a risk of adverse outcomes among people living with HIV who are infected with SARS-CoV-2 compared to those living with HIV who are not infected by the novel coronavirus. The dynamic model will capture how the pandemic shapes and changes over time in people with HIV.
The team, which includes investigators at the University of Washington and Fred Hutchinson Cancer Research Center in Seattle, is examining medical records of people who are living with HIV and have COVID-19 across eight academic centers in the U.S. The data is derived from the CFAR Network of Integrated Clinical Systems (CNICS), a National Institutes of Health-funded research network with access to information from 35,000 patients’ electronic medical records that is collected from the nation’s eight Center for AIDS Research facilities including one at UC San Diego.
1.2 million people were living with HIV in the United States in 2018, according to the CDC. Between 2014 to 2018 the number of new diagnoses increased by 7 percent.
Stigma déja vu
“It’s been difficult,” said Anna. “After the COVID-19 diagnosis, everyone distanced themselves from me. They do not speak to me. It is as though I were just told I had HIV all over again.”
People living with HIV suffer from psychosocial disorders including depression, loneliness, stigma, poverty, homelessness as well as alcohol, drug and tobacco abuse, said Cachay.
“When the response to COVID-19 came, rightfully so, we were asked to social distance,” said Cachay. “Ironically, our patients became more isolated, lonelier than ever, and raised more questions about their health than for the average citizens. It was our patients’ perceptions that inspired us to study the impact of COVID-19 on people with HIV.”
The longer people live with HIV, the higher the risk of developing additional medical complications such as diseases of the kidney, heart and lung. Along with access to healthcare and psychosocial disorders, the combination of these biological factors and social determinants may play a role in the severity of illness as well as the ultimate outcome, said Cachay. He hopes his research will narrow the disparities and help people like Anna.
Thankfully, Anna’s symptoms, while persistent, have not been severe or required hospitalization. But the impact is profound. She wants people to know about the emotional toll the disease and society can have on people with COVID-19.
“Instead of being scared of us or isolating from loved ones, we should be more united—just with added precautions,” said Anna.
Source: Read Full Article
