Non-alcoholic fatty liver disease (NAFLD) in pregnancy has nearly tripled over the past ten years. It increases risks for both mother and baby, including hypertensive complications of pregnancy, bleeding after delivery, and preterm birth, report investigators in the Journal of Hepatology. They recommend that NAFLD should be considered a high-risk condition in pregnancy and that women with NAFLD should receive preconception counseling regarding these risks.
NAFLD is rising in young adults, with potential implications for women of childbearing age. Globally, around 25 percent of all individuals are affected with NAFLD. It is the most common cause of chronic liver disease (CLD) in the United States and includes simple steatosis (accumulation of fat in the liver), as well as hepatocellular injury and fibrosis, known as non-alcoholic steatohepatitis (NASH). NAFLD is considered the hepatic manifestation of the metabolic syndrome and is tightly linked with obesity and diabetes.
The obesity epidemic has affected reproductive-aged women, with obesity present in more than one third of US women aged 20-39 years. Pregnancy itself is a relative insulin resistant state and concurrent maternal obesity further increases the risk for gestational diabetes. The adverse risks of obesity and gestational diabetes on perinatal outcomes are well established, although whether NAFLD is independently associated with more serious pregnancy-related complications is unknown.
“Emerging US data highlight the largest rise in NAFLD incidence among adults under 40 years of age, and NASH is now the leading indication for liver transplantation in young adults,” explained lead investigator Monika Sarkar, MD, University of California, San Francisco, Division of Gastroenterology and Hepatology, San Francisco, CA, USA. “The public health implications of NAFLD and NASH in young adults, including women of childbearing age, are therefore vast. In the current study, we investigate the implications of NAFLD in young women and demonstrate that it does indeed confer distinct risks for their pregnancies, including both maternal and perinatal health.”
Investigators used hospital discharge records from the US National Inpatient Sample database from 2007-2016 to evaluate temporal trends of NAFLD in around 18.5 million women 18 years or older who gave birth after 20 weeks of gestation, including live and stillbirths. Of these women, 5,640 had NAFLD and 115,210 had other, non-NAFLD CLD. Pregnancies with NAFLD nearly tripled from 10.5 of 100,000 pregnancies in 2007 to 28.9 of 100,000 pregnancies in 2015.
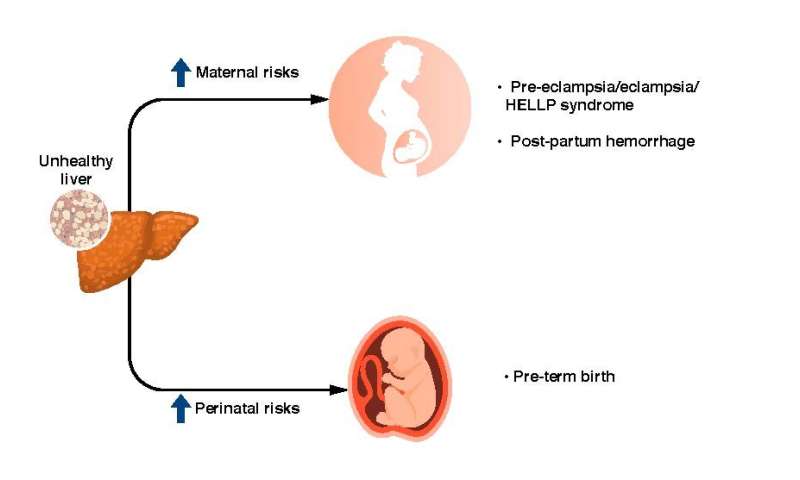
Researchers then evaluated whether having NAFLD in pregnancy was associated with adverse maternal and perinatal outcomes, as compared with other types of CLD and no CLD in pregnancy. They found that NAFLD was associated with hypertensive complications in pregnancy, defined as preeclampsia, eclampsia, and/or HELLP (Hemolysis, Elevated Liver Enzymes, Low Platelets) syndrome, preterm birth, and maternal bleeding after delivery (post-partum hemorrhage), independent of other pre-existing metabolic disease.
“These data support the need for more routine consideration of NAFLD in pregnancy, particularly in women with existing metabolic comorbidities,” commented Dr. Sarkar. “Women with NAFLD warrant preconception counseling regarding maternal and perinatal risks, as well as management by a high-risk obstetrician during pregnancy.
Source: Read Full Article
