University of Illinois Chicago researchers have developed a compound that may one day offer hope for pancreatic cancer treatment.
A pre-clinical study of the experimental compound shows that it more than doubles the average survival time for mice with pancreatic cancer, and that survival time was extended further when combined with immunotherapy.
Led by Ajay Rana, professor of surgery at the UIC College of Medicine and member of the University of Illinois Cancer Center, the study describes the experiments and how the compound—called XP-524—works.
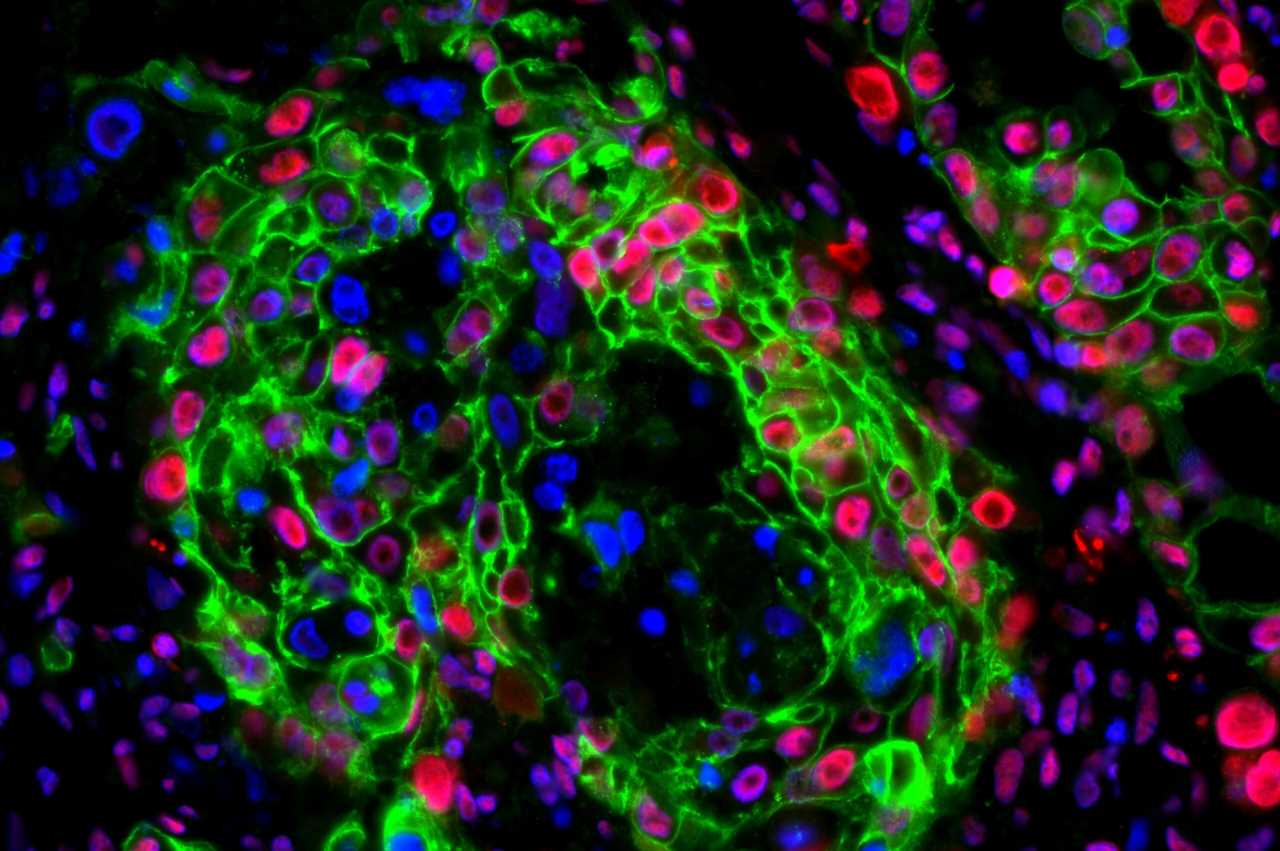
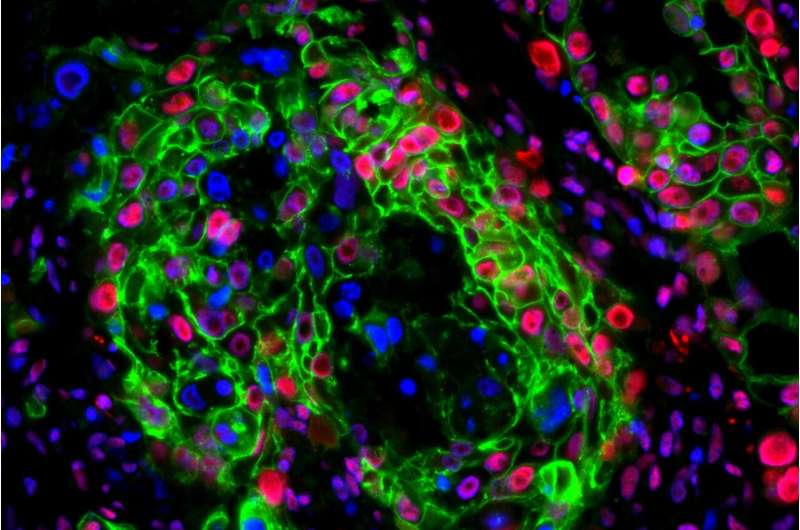
XP-524 alters two proteins involved in the formation of several tumor types—bromodomain and extra-terminal motif (BET) and histone acetyltransferase EP300/CBP (EP300). The compound blocks these proteins, which helps to reactivate immune responses to the most common type of pancreatic cancer, pancreatic ductal adenocarcinoma.
In the study, the researchers found that XP-524 also sensitizes the pancreatic tumors to immune checkpoint therapy, a specific type of immune therapy that helps the body recognize and fight cancer cells.
“In addition to extending survival in laboratory models of the disease, we also found XP-524 turned on the immune response and, when used in combination with an anti-PD1 antibody, more than doubled the median survival time in mouse models,” he said. “It could be a useful strategy to sensitize pancreatic tumors to immune checkpoint inhibition.”
Currently, there are no effective treatments for pancreatic cancer. The disease, which is resistant to chemotherapy, radiation therapy and immunotherapy, has a low five-year survival rate—11% for all stages combined and less than 5% for cancer that has spread. In studies, XP-524 appears to reprogram the pancreatic tumor to extend survival, Rana explained.
“BET inhibitors show promise for treating pancreatic cancer,” Rana said. “By simultaneously targeting two aspects of the disease process, we see the potential for a clinically effective treatment.”
Previously, clinical trials involving other BET inhibitors were stopped due to high toxicity and limited clinical efficacy. However, that data suggested that BET inhibitors may be more effective when combined with other treatments, which led researchers to investigate a combination approach, Rana said.
Source: Read Full Article