Breast screening women aged 40-49 reduces breast cancer mortality, with minimal increased overdiagnosis, according to a study led by Queen Mary University of London that looked at data from 160,000 women.
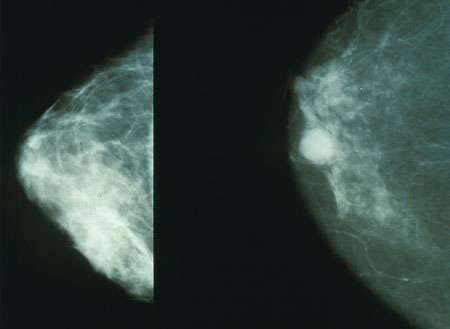
The UK, along with many other countries, has a breast cancer screening programme offering mammography to women aged 50-70 years every 3 years. However, uncertainty currently exists over whether to start screening at a younger age, including whether it might lead to overdiagnosis of breast cancer.
Between 1990 and 1997, the UK Breast Screening Age Trial randomised more than 160,000 UK women aged 39-41 to receive either annual mammography, or the usual NHS breast screening which commences at age 50. The primary outcome was mortality from breast cancers diagnosed prior to first NHS breast screen.
In a new analysis, published in The Lancet Oncology which presents the 23-year follow-up results of the trial, it was found that screening women aged 40-49 led to a substantial and significant 25 per cent reduction in breast cancer mortality in the first ten years. The total years of life saved from breast cancer in the intervention group was estimated as 620, corresponding to 11.5 years saved per 1,000 women invited to earlier screening.
The results also suggest at worst modest overdiagnosis in this age group, and that any overdiagnosed cancers would otherwise be diagnosed at NHS screening from 50 years of age. Therefore, screening in the age group of 40-49 years does not appear to add to overdiagnosed cases from screening at age 50 years and older.
Lead researcher Professor Stephen Duffy from Queen Mary University of London said: “This is a very long term follow-up of a study which confirms that screening in women under 50 can save lives. The benefit is seen mostly in the first ten years, but the reduction in mortality persists in the long term at about one life saved per thousand women screened.
“We now screen more thoroughly and with better equipment than in the 1990’s when most of the screening in this trial took place, so the benefits may be greater than we’ve seen in this study.”
Source: Read Full Article
