Younger patients with resected melanoma had some benefit from adjuvant treatment with the anti-VEGF therapeutic bevacizumab (Avastin) while older patients with resected melanoma did not, according to results published in Clinical Cancer Research, a journal of the American Association for Cancer Research.
Preclinical data showed that VEGF, a protein that promotes angiogenesis and is the target of bevacizumab, decreased with age, and was superseded by the protein sFRP2 in promoting angiogenesis.
“Over the years, it has become increasingly clear that we cannot rely on a one-size-fits-all approach when selecting treatments for patients with cancer,” said Ashani Weeraratna, Ph.D., who is a Bloomberg Distinguished Professor of Cancer Biology and an E.V. McCollum professor and chair in the Department of Biochemistry and Molecular Biology at the Johns Hopkins School of Public Health and professor in the Department of Oncology at Johns Hopkins School of Medicine in Baltimore. “Our work highlights the fact that younger patients can have very different responses to a given therapy compared with older patients. Understanding that the age of a patient can affect response to treatment is critical to providing the best care for all patients.”
Weeraratna and colleagues analyzed data from the phase III AVAST-M clinical trial, which evaluated bevacizumab as an adjuvant treatment among 1,343 patients with resected melanoma. Previous studies demonstrated that treatment with bevacizumab resulted in a slight improvement in disease-free survival compared with those who did not receive bevacizumab. However, these prior analyses did not consider age as a variable, Weeraratna noted.
In their post-hoc trial analysis, Weeraratna and colleagues aimed to determine if there was an interaction between age and response to adjuvant bevacizumab. They found that among younger patients with resected melanoma (those under the age of 45), those who received bevacizumab had significantly longer disease-free survival with a 29 percent decreased risk in disease progression compared with those who did not receive bevacizumab. There was also a 25 percent decreased risk in overall mortality, but this finding was not statistically significant. However, among older patients with resected melanoma (those over the age of 45), there was no significant impact of bevacizumab therapy on disease-free survival or overall survival.
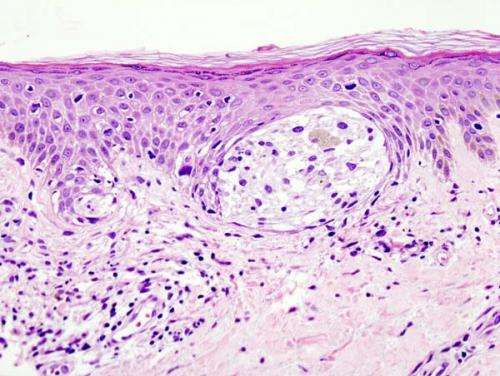
Bevacizumab inhibits the protein VEGF, a cytokine that promotes angiogenesis (the development of new blood vessels), which is a process that facilitates tumor growth. To understand how age impacts angiogenesis, Weeraratna and colleagues analyzed whole tumor samples from young and aged melanoma patients. They found that blood vessel density was significantly increased in patients over the age of 65 compared with those under the age of 65, indicating that aging increases angiogenesis among patients with melanoma. However, when the researchers analyzed age-stratified melanoma samples from The Cancer Genome Atlas (TCGA) database, they found that the expression of both VEGF and its associated receptors were significantly decreased among aged patients.
“This finding was really surprising to us, as we assumed that an increase in angiogenesis would correspond with an increase in VEGF expression among aged melanoma patients,” said Weeraratna.
Because the increase in age-related angiogenesis was not accompanied by increased expression of VEGF, and because older patients with melanoma did not appear to benefit from treatment with adjuvant bevacizumab, the researchers hypothesized that other factors were driving angiogenesis in this patient population. Weeraratna and colleagues performed extensive preclinical analyses and found that the proangiogenic factor sFRP2 (for secreted frizzle-related protein 2) superseded VEGF as the predominant angiogenic factor during aging.
“While sFRP2 levels increase in the aged tumor microenvironment, accounting for the increase in angiogenesis, VEGF levels decrease, which explains why anti-VEGF treatment is no longer effective in older patients with melanoma,” said Mitchell Fane, Ph.D., a postdoctoral fellow in the Weeraratna lab and one of the three lead authors of this study, along with Brett Ecker, MD, and Amanpreet Kaur, Ph.D.
“Our results underscore the importance of considering age in designing preclinical studies, in clinical trial enrollment, and when interpreting trial results,” Weeraratna added.
Source: Read Full Article
