COVID-19 is the disease caused by infection with the SARS-CoV-2 virus. Since it emerged at the end of 2019, the virus has caused a global pandemic. Vaccination against COVID-19 has brought hope, but has also raised questions. EULAR—the European Alliance of Associations for Rheumatology—formed a Task Force to help provide guidance for answering questions around vaccination. The group included patients, health professionals, and rheumatologists with experience in the field of RMDs and vaccination.
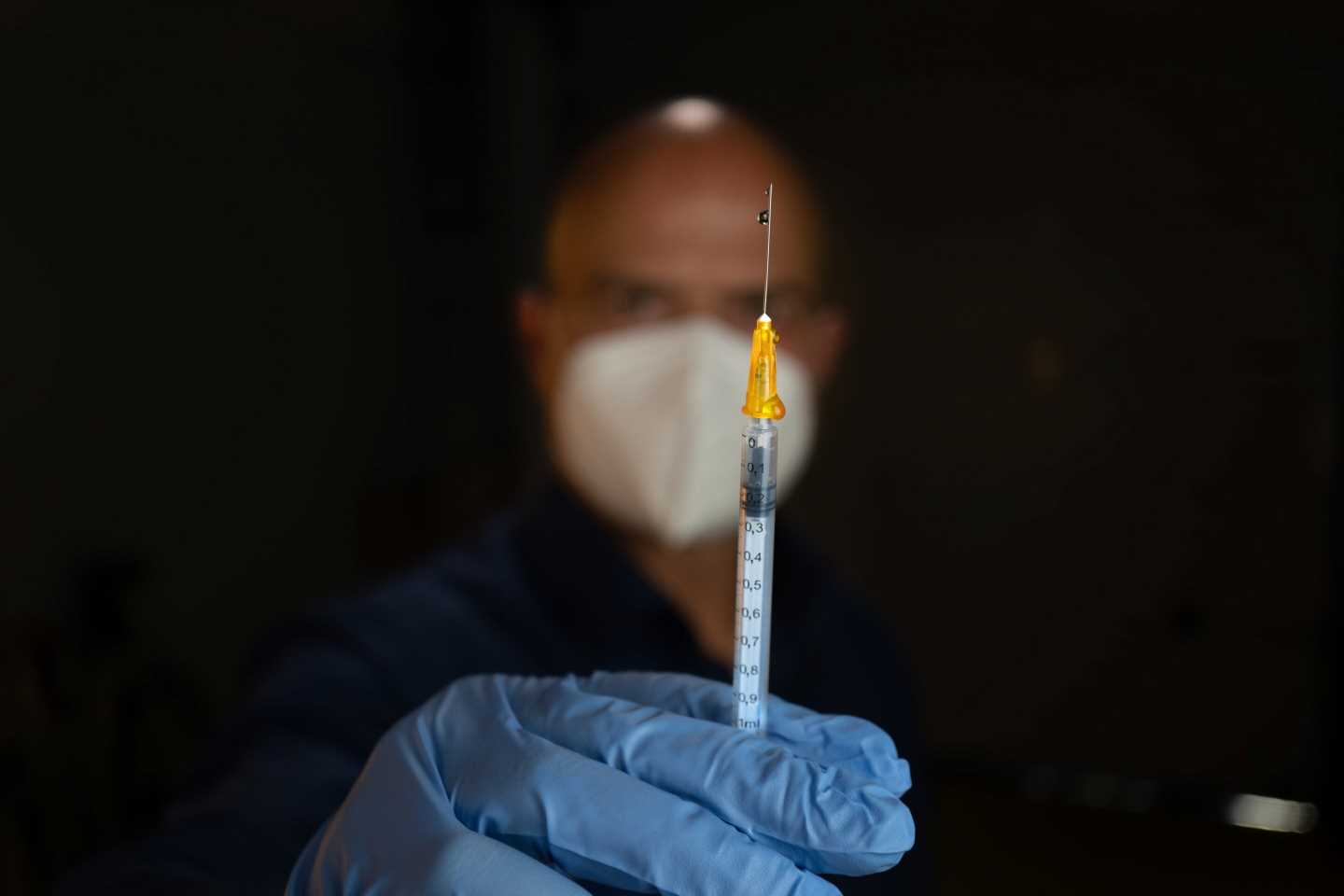
It is important to understand that all vaccines presently being used for COVID-19 are non-live. They cannot cause an infection, or change a person’s genetic information. In addition, there is no evidence that vaccination is a risk to an unborn child. The available COVID-19 vaccines have been shown to be safe in people with RMDs as well as in people receiving drugs that influence the immune system. In other infectious diseases (such as influenza), non-live vaccines have been shown to work for immune-suppressed patients.
The updated EULAR viewpoints, published in ARD, the Annals of the Rheumatic Diseases, provide guidance for answering a selection of over 20 frequently asked questions around vaccination. These cover a range of topics, from the need for vaccination and booster doses, to the choice of vaccine, and risk of side effects and flares. The publication also summarizes the approved vaccines currently available in Europe and provides advice and recommendations for managing people taking drugs that might influence the immune response to COVID-19 vaccination. It is hoped that this important work will raise awareness of vaccination in people with RMDs, and help share critical information to support decision making and prevent infections. Overall, the evidence suggests that there is no reason to withhold vaccines from people with RMDs, or those treated with drugs that influence the immune system.
Questions around vaccination answered in the paper:
- Do I need to be vaccinated?
- Do I need to get a third (supplemental) vaccination?
- Do I need to get a booster vaccination?
- Is one vaccine better for me than another one?
- Can I get COVID-19 and influenza vaccinations together?
- I had COVID-19 and recovered from it. Should I be vaccinated?
- Can I get the vaccination if I take antirheumatic or immunosuppressive drugs?
- Do vaccines interfere with my medication?
- Do I need to measure my antibody response after vaccination?
- Who should I consult before vaccination—my GP or my rheumatologist?
- What data are necessary to take the right decision?
- What about side effects?
- What should I do in case of a flare?
- What should I do if I have side effects that last longer than 48 hours?
- Will I need a vaccination annually as with other vaccinations, e.g., ‘flu?
- What about long-term effects?
- Am I more at risk of getting COVID-19 infection?
- Am I more at risk of getting severe COVID-19 infection?
- Do my treatments increase the risk of severe COVID-19 infection?
- Should I encourage my relatives and friends to get vaccinated?
- Am I fully protected against COVID-19 when I’m vaccinated?
Source: Read Full Article