Researchers in France have discovered that patients suffering from severe COVID-19 show changes in a class of immune cells known as unconventional T cells. The study, published today in the Journal of Experimental Medicine (JEM), suggests that monitoring the activity of these cells in the blood of patients could predict the severity and course of the disease.
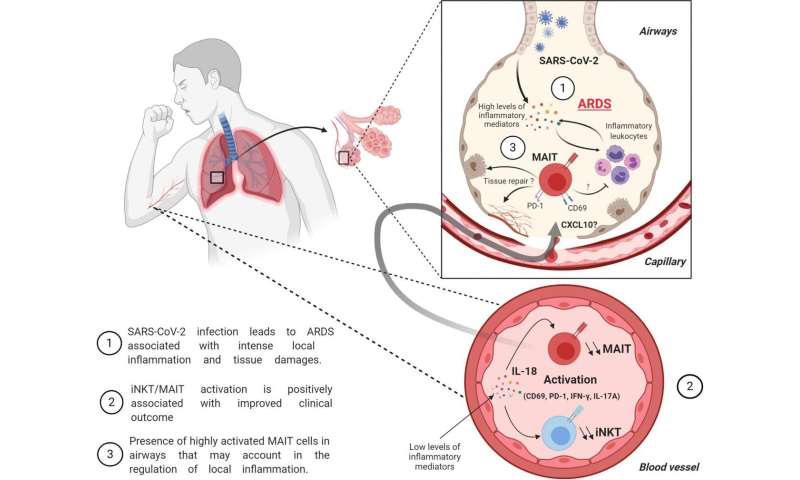
While most people infected with the SARS-CoV-2 virus experience relatively mild symptoms, some patients mount an aberrant inflammatory response that can damage the lungs and cause acute respiratory distress syndrome (ARDS), potentially resulting in the patient’s death. However, the immune cells and inflammatory molecules responsible for ARDS associated with COVID-19 remain unclear.
Unconventional T cells are a diverse class of immune cells that help control the response to viral infection and are commonly found in the lungs and other mucosal tissues in the body. “Despite this, the role of unconventional T cells in the pathophysiological process of SARS-CoV-2-driven ARDS has not yet been explored,” says Christophe Paget, a researcher at the INSERM Research Center for Respiratory Diseases, University of Tours.
Paget and colleagues, including co-lead author Youenn Jouan, an intensivist at the academic hospital of Tours, examined 30 patients admitted to intensive care with severe COVID-19 and compared the immune cells in their blood and lungs to those found in healthy volunteers or patients admitted to the ICU for reasons other than COVID-19.
The researchers found that two types of unconventional T cells—known as mucosal-associated invariant T (MAIT) and invariant natural killer T (iNKT) cells—were dramatically reduced in the blood of patients with severe COVID-19. However, the number of MAIT cells increased in the patients’ airways, suggesting that these cells might move from the blood to the lungs to control the response to SARS-CoV-2 infection.
The MAIT and iNKT cells of COVID-19 patients appeared to be highly activated and produced distinct sets of inflammatory molecules. The researchers found that patients whose circulating MAIT and iNKT cells were particularly active at the time of their admittance to the ICU were less susceptible to hypoxemia (low blood oxygen levels) and were discharged sooner than patients whose MAIT and iNKT cells were less active.
“This suggests that MAIT and iNKT cells might play a beneficial role during severe COVID-19, although their precise functions and associated mechanisms require further investigation,” says Jouan.
Source: Read Full Article
