In a review article published in the journal Signal Transduction and Targeted Therapy, scientists have discussed host metabolic alteration triggered by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its effect on disease severity.
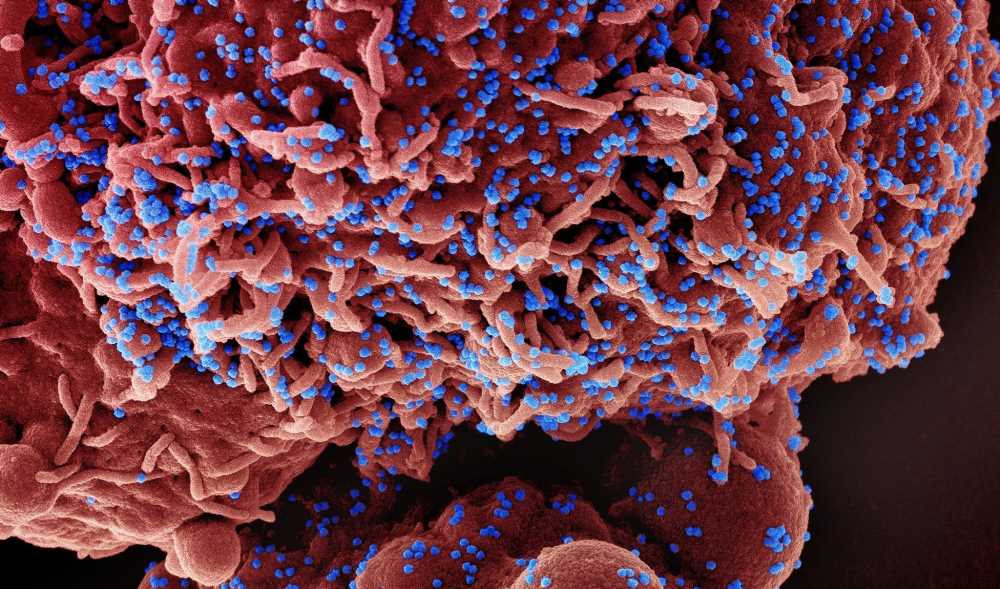
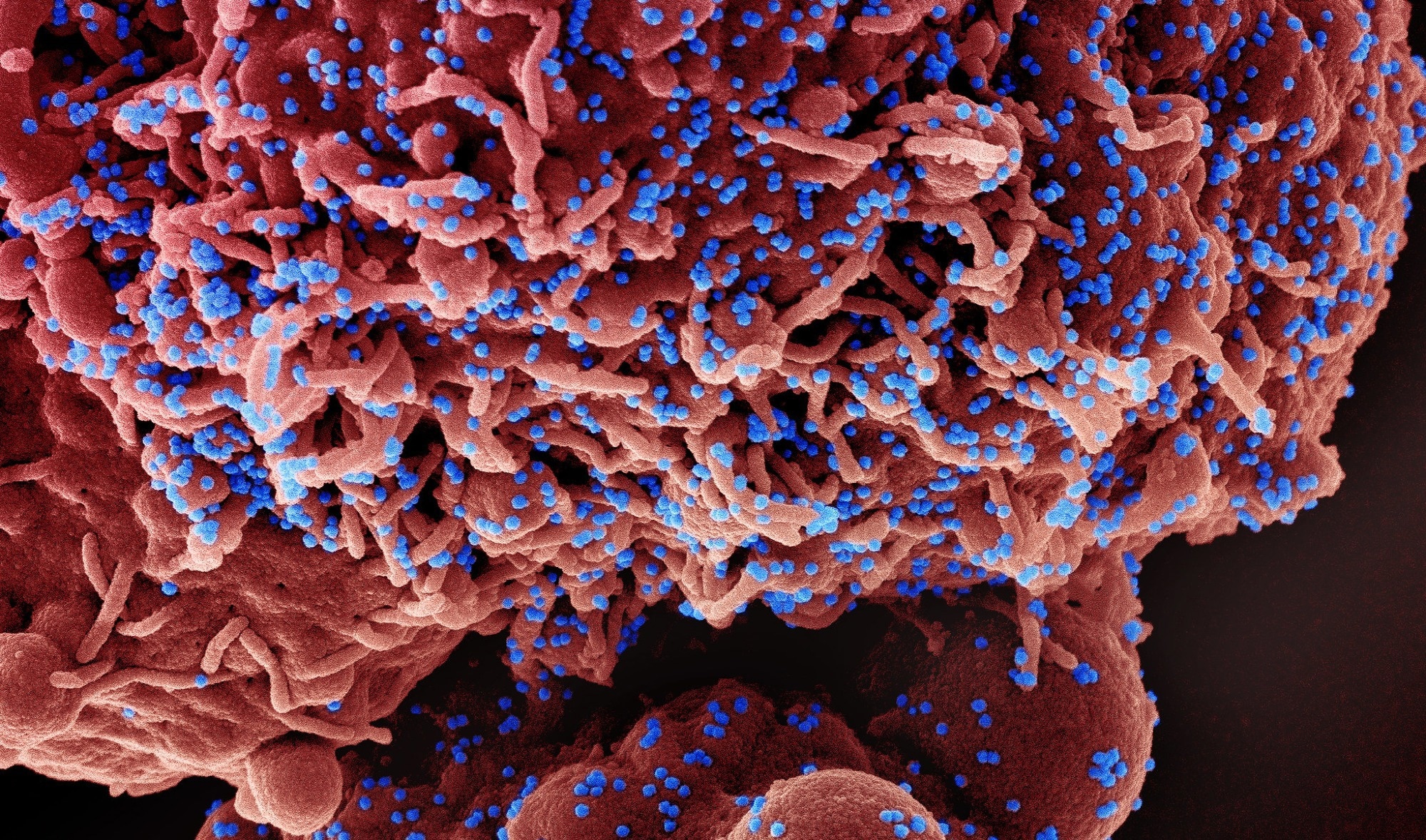 Study: Metabolic alterations upon SARS-CoV-2 infection and potential therapeutic targets against coronavirus infection. Image Credit: NIAID
Study: Metabolic alterations upon SARS-CoV-2 infection and potential therapeutic targets against coronavirus infection. Image Credit: NIAID
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen of coronavirus disease 2019 (COVID-19) pandemic, is an enveloped positive-sense, single-stranded RNA virus belonging to the human beta-coronavirus family. The virus enters host cells by interacting with the host cell membrane receptor angiotensin-converting enzyme 2 (ACE2) through its surface glycoprotein, the spike protein.
Host metabolism plays vital a role in regulating various physiological processes during viral replication. Conversely, many viruses can modulate host metabolism to support their lifecycle within host cells and evade host immune responses.
Studies have shown that viruses can alter host lipid metabolism to create replication compartments. In COVID-19 patients, an accumulation of lipids has been observed in the lungs. Lipid pattern alterations induced by SARS-CoV-2 have been found to associate with disease severity.
Type 2 diabetes has been identified as one of the significant risk factors for severe COVID-19 and mortality. Increased glycolysis has been observed in all immune cells in COVID-19 patients. These observations highlight an association between SARS-CoV-2 infection and glucose metabolic alteration.
SARS-CoV-2 host cell entry
The interaction between spike protein and ACE2 through the spike S1 domain leads to the cleavage of spike protein by host transmembrane protease TMPRSS2 at the S2 site. This is followed by the fusion of the viral envelope and host lipid bilayer and the release of viral particles into host cells.
Lipid rafts are microdomains containing lipid molecules, including cholesterols and sphingolipids. Evidence shows that lipid rafts located at the host cell membrane play crucial roles in the SARS-CoV-2 entry process by providing platforms for membrane receptors. Lipid rafts can also support cell-to-cell viral transmission by facilitating syncytia formation. Lipid raft disruption induced by cholesterol trafficking from the membrane to the endoplasmic reticulum (ER) has been found to reduce SARS-CoV-2 host cell entry.
SARS-CoV-2 spike protein can directly bind to cholesterol and receptor-bound high-density lipoprotein (HDL). The spike protein has been found to capture lipid components from cell membranes by bindings to and altering the function of HDL.
As with membrane cholesterol, intracellular cholesterol is also involved in viral entry. Genetical screening by CRISPR libraries have identified certain genes related to cholesterol metabolism that are essential for SARS-CoV-2 infection.
Various sphingolipids, especially ceramide, and sphingosine, play prominent roles in SARS-CoV-2 host cell entry. Ceramide is converted from sphingomyelin by acid sphingomyelinase (ASM) or synthesized de novo from palmitoyl CoA and serine. Ceramide has been found to facilitate SARS-CoV-2 entry by forming ceramide-rich microdomains where ACE2 clusters. Several ASM inhibitors have been found to prevent SARS-CoV-2 entry by altering surface ceremide levels.
Sphingosine is derived from ceramide by ceramidase catalyzation or sphingosine 1-phosphate (S1P) by S1P phosphatase catalyzation. In contrast to ceremide, sphingosine has been found to prevent viral entry by binding to ACE2 and blocking the spike-ACE2 interaction. S1P, a downstream product of sphingosine, has also been found to improve COVID-19 clinical presentation by protecting the endothelial barrier.
Modification of SARS-CoV-2 spike protein
Evidence shows that the SARS-CoV-2 entry process can be regulated by lipid-mediated post-translational modification of the spike protein. The binding of linoleic acid to the spike protein has been found to lock the protein in a closed conformation, leading to the inhibition of viral entry.
In contrast, covalent attachment of fatty acids to the spike protein (palmitoylation) has been found to promote viral entry by stabilizing the spike protein homotrimer. Spike protein palmitoylation is a conserved process across all coronaviruses.
In type 2 diabetes, high blood glucose level has been found to promote viral entry by increasing ACE2 expression. In addition, spike protein glycosylation (covalent attachment of sugar moieties) has been found to modulate the viral entry process significantly.
SARS-CoV-2 replication
Besides viral entry, host lipids modulate SARS-CoV-2 replication. Studies have shown that glycerophospholipid metabolism promotes viral replication by triggering the formation of double-membrane vesicles.
Recent evidence has shown that SARS-CoV-2 utilizes host lipid droplets to meet the energy demand of replication. TMEM41B, an ER-localized protein responsible for lipid mobilization from lipid droplets, has been identified as a vital host factor for SARS-CoV-2 replication.
Like many other viruses, SARS-CoV-2 induces the “Warburg effect” (a shift of glucose metabolism to aerobic glycolysis) to facilitate replication. Glycolysis provides energy and building blocks for nucleotide synthesis, which are prerequisites for viral replication.
One carbon metabolism also facilitates SARS-CoV-2 replication by providing materials for RNA capping, which is required for preventing RNA degradation by innate immune responses and facilitating viral protein translation.
SARS-CoV-2 assembly
Host lipids play important roles in SARS-CoV-2 assembly. Studies have shown that viral membrane protein uses several lipid components to induce membrane curvature. Similarly, palmitoylation has been found to support viral assembly by stabilizing envelop protein and maintaining its functional architecture.
Drug repurposing
Considering the significant involvement of host metabolism in SARS-CoV-2 infection, several lipid-modulating and glucose-modulating drugs, including statins, ASM inhibitors, non-steroidal anti-inflammatory drugs, montelukast, omega-3 fatty acids, 2-deoxy-D-glucose, and metformin, have been repurposed to manage COVID-19. These drugs are currently under clinical investigation for treating COVID-19 patients.
- Chen P. 2023. Metabolic alterations upon SARS-CoV-2 infection and potential therapeutic targets against coronavirus infection. Signal Transduction and Targeted Therapy, https://www.nature.com/articles/s41392-023-01510-84
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Anti-Inflammatory, Blood, Cell, Cell Membrane, Cholesterol, Coronavirus, Coronavirus Disease COVID-19, CRISPR, Diabetes, Drug Repurposing, Drugs, Enzyme, Fatty Acids, Genes, Glucose, Glucose Metabolism, Glycolysis, Glycoprotein, Glycosylation, Intracellular, Linoleic Acid, Lipids, Lipoprotein, Lungs, Membrane, Metabolism, Metformin, Mortality, Nucleotide, Pandemic, Pathogen, Phosphatase, Protein, Receptor, Respiratory, RNA, SARS, SARS-CoV-2, Serine, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Translation, Type 2 Diabetes, Virus

Written by
Dr. Sanchari Sinha Dutta
Dr. Sanchari Sinha Dutta is a science communicator who believes in spreading the power of science in every corner of the world. She has a Bachelor of Science (B.Sc.) degree and a Master's of Science (M.Sc.) in biology and human physiology. Following her Master's degree, Sanchari went on to study a Ph.D. in human physiology. She has authored more than 10 original research articles, all of which have been published in world renowned international journals.
Source: Read Full Article