When people think about the connection between genes and disease, they often envision something that works like a light switch: When the gene is normal, the person carrying it does not have the disease. If it gets mutated, a switch is flipped, and then they do have it.
But it’s not always that simple. Disease-related genes often have different degrees to which they are turned on or off. In these cases, there is a tipping point: With only an incremental biological change around a critical threshold, a person can go from having no symptoms to being very sick. The latest research on this topic from the Salk Institute has implications for studying and treating the underlying causes of amyotrophic lateral sclerosis (ALS) and other neurological and psychiatric disorders. The work, which was published in Neuron on August 26, 2021, could also be applicable to a wide range of diseases involving changes in gene expression levels, like cancer.
“This is increasingly becoming a new and very interesting direction for ALS research,” says Salk Professor Samuel Pfaff, the paper’s senior author. “Our study is highly revealing in terms of how gene regulation occurs within neurons. While our experiments were done in mice, we believe these findings will also apply to humans.”
A handful of genes has been found in patients that are associated with ALS, a disease of the motor neurons that leads to paralysis. What many of these genes have in common is that they are linked to the manufacture of microRNAs (miRNAs)—regulatory molecules that act like brakes to reduce the production of proteins. In the first part of this research, the team did a systematic review of past studies that profiled microRNA levels in patients with ALS. They found that across all the studies, the same microRNA, called miR-218, kept showing up as being lower, but not completely lost, in people with ALS. They decided to study why particular levels of miR-218 are important for motor neurons to do their job normally.
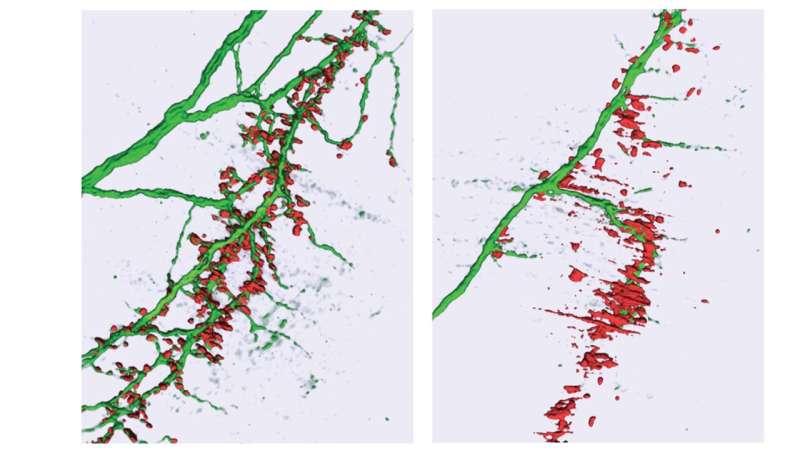
In a mouse model of ALS, Salk researcher Neal Amin, now a clinical scholar and postdoctoral researcher at Stanford University, devised a strategy to finely lower the levels of miR-218 in a controlled way to study the effects on motor neurons’ control of muscle function. Amin found that there’s a critical threshold somewhere between 36 percent and 7 percent of normal levels that leads to muscle paralysis and death. Above 36 percent, neuromuscular junctions are normal and healthy; below 7 percent, neuromuscular deficits are lethal. The rest of the study was focused on trying to understand why that was the case.
It turns out that miR-218 regulates the function of about 300 different genes. Many of them encode proteins related to how motor neurons grow axons and send signals to muscle. Once the levels of miR-218 dropped below 36 percent, the way these neurons could signal to muscles dropped off dramatically. The researchers used cutting-edge tools in the lab to determine how miR-218 was influencing various genes.
“Instead of acting like a simple switch, the molecule miR-218 is like an orchestra conductor of 300 musicians playing together,” Amin says. “Instead of gradually telling all of the players to dim the volume of their instruments in unison, it’s telling some musicians to play more quietly and others to stop completely. It has a much more dynamic and complex control over gene function than we ever previously appreciated.”
The researchers say that being able to study this fine-tuning in animal models will allow them to learn much more about how genetic mutations that reduce gene expression put patients at risk for developing brain disorders. This could eventually lead to new treatments that get at the heart of the biological changes that lead to disease. The research not only has implications for ALS, but for other diseases of the nervous system, including schizophrenia, which has also been associated with changes in the expression level of microRNAs.
Source: Read Full Article
