Long COVID patients have clear differences in immune and hormone function to patients without the condition, according to a new study led by the Icahn School of Medicine at Mount Sinai and Yale School of Medicine.
The research, published in the September 25 issue of Nature, is the first to show specific blood biomarkers that can accurately identify patients with long COVID.
“These findings are important—they can inform more sensitive testing for long COVID patients and personalized treatments for long COVID that have, until now, not had a proven scientific rationale,” says Principal Investigator David Putrino, Ph.D., Professor of Rehabilitation and Human Performance and Director of the Abilities Research Center at Icahn Mount Sinai, and the Nash Family Director of the Cohen Center for Recovery From Complex Chronic Illness.
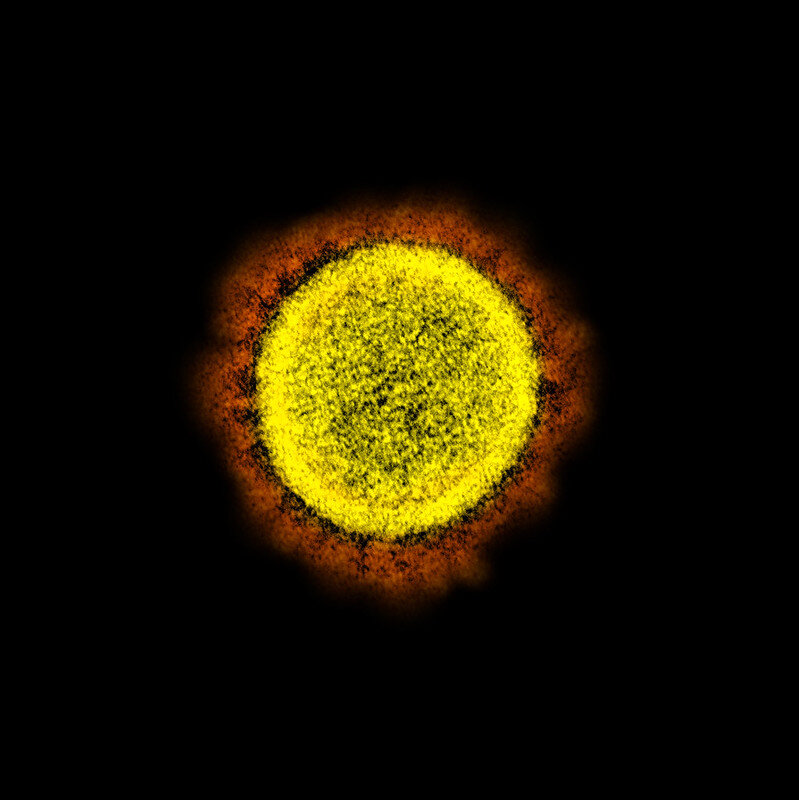
“This work is so exciting because it is one of the first to show us clear, measurable differences in blood biomarkers of people with long COVID compared with people who recovered fully from an acute infection and a group of people who have never been infected with SARS-CoV-2 (the virus that causes COVID-19). This is a decisive step forward in the development of valid and reliable blood testing protocols for long COVID.”
Physicians from the Mount Sinai Health System first identified long COVID symptoms in 2020 when patients reported persisting issues after an initial, diagnosed case of COVID-19. These symptoms included cognitive impairment or “brain fog,” extreme fatigue, shortness of breath, and chronic pain.
The Centers for Disease Control and Prevention says 1 in 13 adults (or 7.5%) in the United States has long COVID symptoms lasting more than three months after having COVID-19. Many of these patients have no clear cause for their symptoms, and this study provides new evidence for why these may exist.
Investigators analyzed a total of 271 patients from three sites—The Mount Sinai Hospital, Mount Sinai Union Square and Yale School of Medicine—between January 2021 and June 2022.
Researchers divided them into three groups: those with no prior SARS-CoV-2 infection; those who had fully recovered from a clinically confirmed case of COVID-19; those with active long COVID symptoms for at least four months or more after confirmed COVID-19 infection (median time of long-term symptoms was 12 months since the acute infection).
Each patient was asked to complete a detailed set of questionnaires about their symptoms, medical history, and health-related quality of life. The researchers took blood samples from all patients, identified biomarker differences and similarities between the groups, and then applied machine learning analyses to better understand which biomarkers were most effective in allowing the algorithm to identify patients with long COVID.
Overall, the algorithm was able to differentiate between people with and without long COVID with 96% accuracy and detect the condition based on distinctive features detected in the blood of participants in the long COVID group.
Some of the most pronounced differences between the long COVID group and the two control groups were related to immune and hormonal dysfunction. This was characterized by biomarkers indicating abnormal T cell activity, reactivation of multiple latent viruses (including the Epstein-Barr virus and other herpes viruses) and significant reductions in cortisol levels.
“These findings show us that people with long COVID are living with a disease process that is observable using the blood testing protocols laid out in the study, but also varies from patient to patient depending on their specific medical history,” says Dr. Putrino.
“This means that physicians must listen to their patients and perform a wide variety of physiological and lab tests, while adopting a highly personalized approach to the medical management of long COVID. There is no ‘silver bullet’ for treating long COVID, because it is an illness that infiltrates complex systems such as the immune and hormonal regulation. Complex illnesses require complex treatment solutions and we need more rapid research to better understand long COVID and discover new and promising therapies.”
“We are excited to see such clear differences in the immune phenotypes in people with and without long COVID. These markers need to be validated in larger studies, but provide a first step in dissecting the disease pathogenesis of long COVID,” adds co-Principal Investigator Akiko Iwasaki, Ph.D., Sterling Professor of Immunobiology and of Molecular, Cellular & Developmental Biology at Yale School of Medicine.
More information:
Distinguishing features of Long COVID identified through immune profiling, Nature (2023).
Journal information:
Nature
Source: Read Full Article