The incidence of overdose-related cardiac arrests more than doubled in King County, Washington, from 2015 to 2021, with the biggest increase among people who had consumed opioids combined with stimulants, according to a new study. That drug profile was also the most lethal among four profiles evaluated.
The findings are troubling because emergency medical responses to drug overdoses are surging in communities across the United States, the authors wrote. The paper was published today in JAMA Network Open.
“Drug abuse and overdose are expanding public health emergencies. Recent reports suggest that the patterns and types of drug use are changing, with many overdoses involving more than opioids alone,” said the lead author, Dr. Neal Chatterjee, a cardiologist and electrophysiologist at the UW Medicine Heart Institute in Seattle.
In medical reports, most out-of-hospital cardiac arrests (OHCA) that involve a drug overdose are recorded simply as “OD” without identifying specific drugs or drug types. In this study, the investigators compared OD-related cases against those not OD-related, and also worked with the medical examiner to differentiate the drug-involved cases into four subgroups: opioid-only, stimulant-only, opioid combined with stimulant, and other nonopioid, nonstimulant drugs.
Opioids included fentanyl, heroin, hydromorphone, methadone, opium, codeine and oxycodone. Stimulants included amphetamines, methamphetamines and cocaine.
The primary outcome measure for all groups was survival to hospital discharge.
During the span (Jan. 1, 2015, to Dec. 31, 2021), King County emergency medical providers responded to 6,790 calls in which someone had experienced cardiac arrest. Of those, 702 (10%) were later determined to have involved a drug overdose.
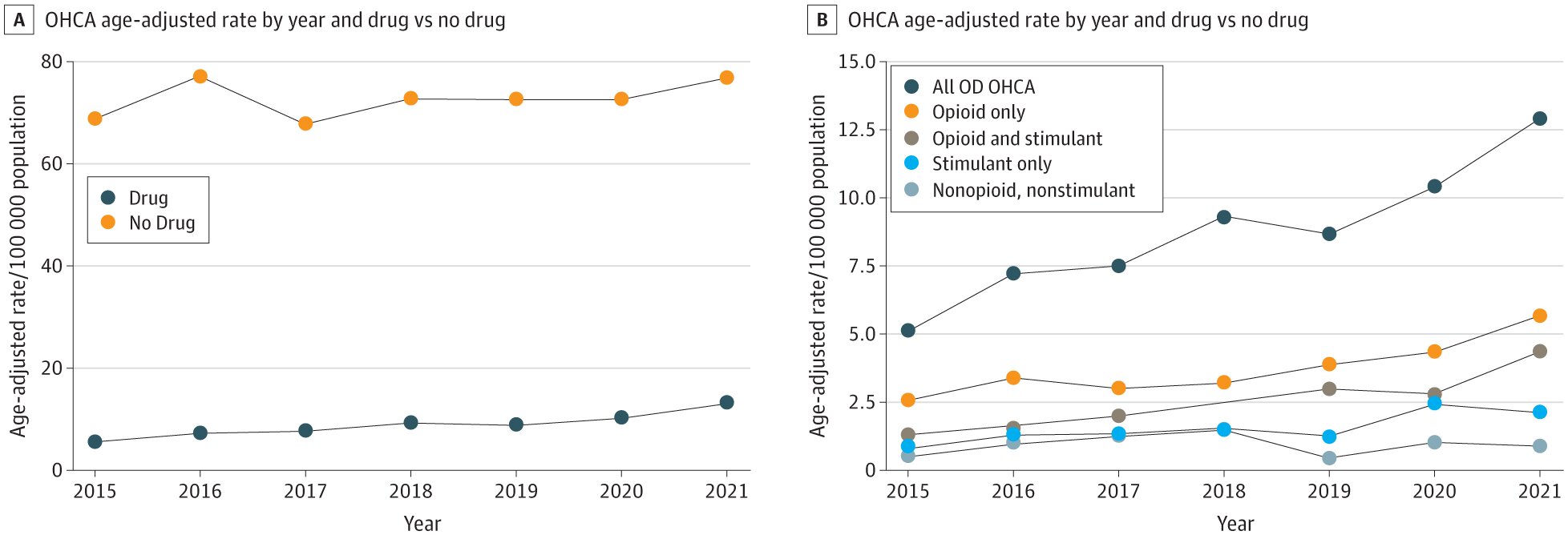
Chatterjee and colleagues found that King County’s incidence of OD-involved OHCA had more than doubled during the six-year span, with no corresponding increase in the incidence of OHCA not involving OD.
At the end of 2021, although opioid-only was the drug profile most commonly involved in OHCA, the combined opioid+stimulant profile had grown to nearly the same incidence, the paper reported. Chatterjee said this finding lends context to the drumbeat of reports characterizing opioids, in particular fentanyl, as the main public health threat.
The opioid+stimulant mix also was associated with worse survival than opioids alone or stimulants alone. Chatterjee hypothesized that this might be due to the dual-organ impact of opioids, which primarily affect the respiratory system, and stimulants, which can increase the risk of cardiac arrhythmias.
“I think our study provides important context when counseling and caring for individuals who use illicit drugs,” he said. “For example, recent qualitative survey data suggests that some of what may be driving an increase in mixed illicit drug use is the misperception that stimulants can improve the safety of, or enhance the high associated with, depressants such as opioids.
“Given our findings that mixing these drugs was associated with the lowest survival in cardiac arrest cases, our study enables those who work in addiction medicine to highlight these dangers.”
Chatterjee also said the study findings do not suggest that emergency responders’ highly orchestrated resuscitation protocols should change when a cardiac arrest case is suspected to be related to drug overdose.
“There is not currently an established resuscitation protocol specific to OD-related OHCA,” he said. “Contemporary guidelines recommend agents like naloxone (to reverse opioid overdose) only after a pulse is restored, but not as part of the primary resuscitation protocol. The chance of surviving after OHCA is about 10%, on average, which indicates lots of room for improvement. Whether tailored resuscitation protocols for OD-OHCA could improve outcomes is an area of future study.”
More information:
Vidhushei Yogeswaran et al, Presentation and Outcomes of Adults With Overdose-Related Out-of-Hospital Cardiac Arrest, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.41921 jamanetwork.com/journals/jaman … /fullarticle/2811464
Journal information:
JAMA Network Open
Source: Read Full Article