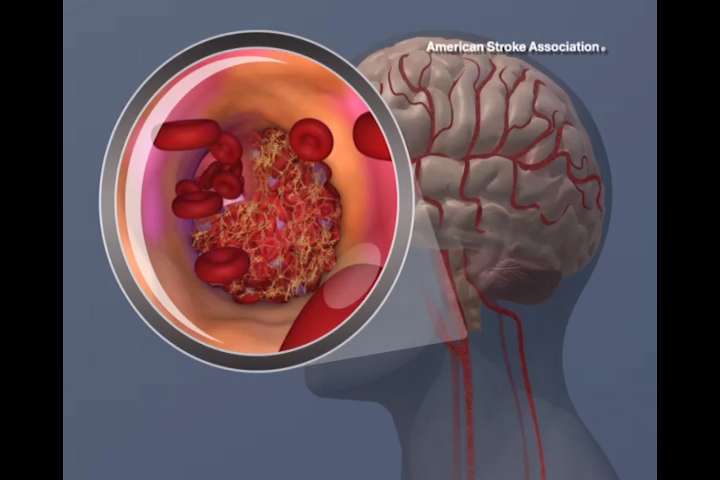
The rate of cardiovascular risk factors among Hispanic/Latino people living in the U.S. is very high, and while they are often aware of their health conditions, less than half of the Hispanic/Latino adults with history of stroke or transient ischemic attack (TIA) had healthy blood pressure and cholesterol, and about half had healthy blood sugar levels, according to new research published today in Stroke, a journal of the American Stroke Association, a division of the American Heart Association.
According to the American Heart Association, from 2015 to 2018, 52.3% of Hispanic men and 42.7% of Hispanic women aged 20 years and older had cardiovascular disease (CVD).
“It’s a wake-up call for the medical community. Despite our best efforts, Hispanic and Latino populations still seem to be undertreated for their vascular risk factors,” said Fernando D. Testai, M.D., Ph.D., FAHA, study co-author and an associate professor of neurology at the University of Illinois at Chicago. “I didn’t expect the numbers to be so dismal. We found many of the participants with previous stroke knew about their vascular risk factors; however, the data indicate they are receiving inadequate treatment and support, which are a real concern.”
Researchers reviewed data from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), a longitudinal study of the health of people of Cuban, Dominican, Mexican, Puerto Rican, and Central and South American background. Between 2008 and 2011, more than 16,000 participants, ages 18 to 74, completed questionnaires about their health and were examined at one of four centers in Chicago, the Bronx neighborhood of New York City, Miami and San Diego.
Drawing from the HCHS/SOL data, researchers focused on data for 404 adults (39% male) who had a self-reported history of stroke or TIA. They investigated the rates of high blood pressure, diabetes and high cholesterol, and assessed whether the 404 study participants knew that they had these major cardiovascular risk factors and the treatment status for these chronic health conditions. They also analyzed if participants were taking medications to prevent a second stroke.
Researchers found:
- Overall, 59% of participants had high blood pressure, 65% had high cholesterol and more than one-third had diabetes (Type 1 or Type 2).
- Even though up to 90% of study participants knew they had these CVD risk factors, most did not have healthy levels: almost half had normal blood pressure levels; one-third had healthy cholesterol levels; and about half had their blood sugar in a healthy range.
- About half of participants were taking anti-clotting medications; less than half were taking cholesterol-lowering statin medications; and one-quarter were taking both medications, the mainstay of stroke prevention.
- Older age was associated with uncontrolled high blood pressure and diabetes.
- Adults born in the U.S. or who have lived in the U.S. more than 10 years were more likely to have poorly controlled diabetes.
- Women were more likely to have unhealthy cholesterol levels; and
- Not having health insurance was associated with decreased statin use and unhealthy cholesterol levels.
“Health care professionals can help inform and support Hispanic/Latino adults about the importance of adopting healthy lifestyle behaviors in order to reduce cardiovascular risk,” Testai said. “Almost 80% of people in this study were overweight or obese, and a significant number continued to smoke despite having a history of stroke and other cardiovascular events. Access to care is another important area that we need to address to reduce cardiovascular risk in this population.”
In this analysis, researchers referenced older guidelines with higher thresholds for healthy blood pressure and cholesterol levels. “We were conservative in our goals. If we used the newer goals, which are far more stringent, the results would be even more alarming,” Testai said.
A major limitation of this study is that HCHS/SOL data was self-reported by participants. Another limitation is that while race was self-reported, social determinants of health and the health impacts of structural racism were not accounted for in this analysis.
The American Heart Association’s November 2020 Presidential Advisory, “Call to Action: Structural Racism as a Fundamental Driver of Health Disparities,” declared structural racism a cause of poor health and premature death from heart disease and stroke for many and detailed the Association’s immediate and ongoing action to accelerate social equity and health care and outcomes for all people.
Source: Read Full Article
