A machine-learning model can identify patients at risk of a rare cardiomyopathy, according to a study published in Nature Communications.
Transthyretin amyloid cardiomyopathy (ATTR-CM) can cause heart failure and should be treated differently than other causes of heart failure, so diagnosis is key, according to Sanjiv Shah, ’00 MD, the Neil J. Stone, MD, Professor, director of the Center for Deep Phenotyping and Precision Therapeutics at the Institute for Augmented Intelligence in Medicine and senior author of the study.
“If we can flag patients in EMR and trigger clinicians to order screening tests, we can diagnose ATTR-CM earlier and get it treated more quickly,” said Shah, who is also a professor of Medicine in the Division of Cardiology.
ATTR-CM is caused by defects in transthyretin, one of the most common proteins in the body. Normally, transthyretin is present in a tetramer—a set of four proteins bound together—and the complexes help transport hormones and vitamins throughout the body.
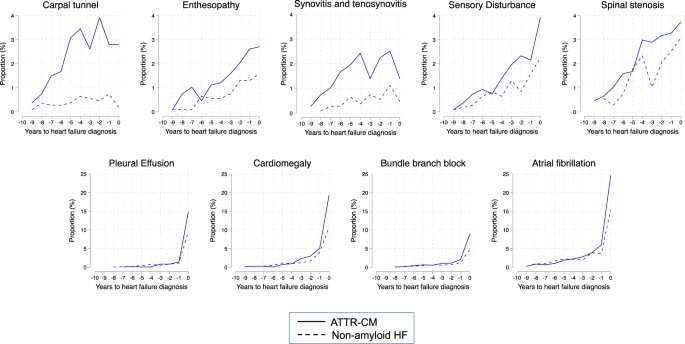
In some individuals, however, due to genetic or age-related factors, the tetramer dissociates, and the individual proteins aggregate and form fibrils. These fibrils deposit into tissues, mainly the heart (contributing to cardiomyopathy), but also in other specific locations including the lumbar spine and the carpal tunnel in the wrist (predisposing those individuals to lumbar spine stenosis or carpal tunnel syndrome, respectively).
ATTR-CM is underdiagnosed, according to Shah, so in the current study, the investigators analyzed a large database of medical claims data to develop a machine learning model to identify ATTR-CM from electronic medical records.
In collaboration with Rahul Deo, MD, Ph.D., associate professor of Medicine at Brigham and Women’s Hospital and a co-author of the study, the investigators trained the model using two datasets; one group of heart failure patients with ATTR-CM and another group of patients without ATTR-CM. This allowed the model to deduce what combination of clinical diagnostic codes were most strongly associated with ATTR-CM.
The strongest associations were pericardial effusion and atrial flutter, and non-cardiac predictors included carpal tunnel and inflamed joints.
Next, the investigators validated the model in additional large medical claims datasets, and eventually tested the final model in EMR data from Northwestern Medicine in collaboration with the Northwestern Medicine Enterprise Data Warehouse (NMEDW).
Predicting presence of ATTR-CM based on unique combinations of clinical features improved sensitivity and specificity of detection, according to the study. Notably, the non-cardiac features could serve as an important clinical mark to distinguish ATTR-CM heart failure from heart failure caused by other conditions, according to Shah.
“If a heart failure patient presents with spine, joint and tendon problems, that may be a hint that the patient has ATTR-CM,” Shah said.
Using medical claims data, rather than echocardiograms or unstructured notes, means this model is generalizable to hospitals across the country. Further, this methodology could be applied to other rare conditions as well, according to Shah.
“It provides us a way to diagnose the disease earlier, but it also helps us identify manifestations of the disease we didn’t previously know about,” Shah said.
Source: Read Full Article
