Talking about a virus is all a lot of us seem to be doing at the moment. We’re happy enough chatting away about COVID-19 and other common viruses like the cold or flu, so why is there so little conversation about HPV?
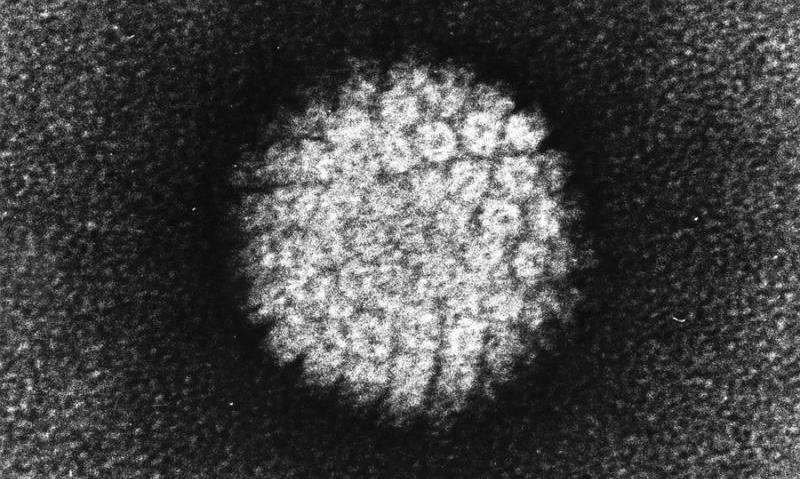
You may have heard about HPV, human papillomavirus, as the virus linked to cancer. Cervical cancer is the type most strongly linked to HPV infection, but HPV can also cause cancer of the anus, penis, vagina and vulva, and some types of mouth and throat cancers. But although HPV can cause cancer, having HPV doesn’t mean you have or will definitely get cancer.
Although not everyone will be comfortable talking to their friends or partners about HPV, our Cancer Research UK nurses have received lots of questions from people worried about what HPV is, and what having HPV means for their health, their partner’s health and very often, their sex life.
You’ve asked and we’ve answered.
Is HPV a sexually transmitted infection?
HPV is a really common virus—most of us will have HPV at some point in our lifetime without it causing any harm and a lot of the time without us knowing.
HPV lives in the skin and the cells lining the inside of our body, so it can pass between people through close skin to skin contact, often during sex. This includes penetrative vaginal and anal sex, oral sex, touching and using sex toys with a partner, such as vibrators or butt plugs.
Labeling HPV as an STI isn’t particularly helpful in a lot of cases. It prompts questions like ‘where did I get it?” or ‘who gave it to me?”, which in reality is not how it works and only adds to the reasons why we don’t want to talk about it.
Having HPV is not something to be ashamed of, and it’s not a sign that you or your partner have been unfaithful. Having HPV is just a totally normal part of life.
How did I get HPV and can I get rid of it?
Now we know how HPV can be passed between people, let’s talk a bit more about how the virus works.
HPV has a ‘dormancy’ period, which means that the virus spends some time in our body without causing any harm, this is usually a couple of years but can stretch to decades.
When HPV is dormant it can’t be detected by a test, but it can become active later which is when it would be picked up in cervical screening. This is also why you might not have had HPV show up in your previous screening but it has in your most recent one—it’s not necessarily that you have had a new HPV infection between screens, but that it has been dormant in your cells.
It’s hard to know how long an infection has been there for if it’s been dormant, so there’s usually no point trying to work out where you ‘got’ HPV.
There’s no cure for HPV but most of the time our body’s immune system does the job and clears up the infection by itself before it’s done any harm. It’s only when certain types, or strains, of HPV can’t be cleared up by our body that damage can happen to our cells. Regular cervical screening monitors HPV infection, it sees if the infection has cleared from your last screen or whether the infection has caused the cells in the cervix to change and need treating.
If I’ve had HPV once can I get it again?
There are over a hundred different types, or strains, of HPV and around 13 of these are linked to cancer. So it’s possible to have multiple infections and you might have different strains of HPV over the years that are picked up at cervical screening.
What the science is less clear on is reinfection—this means getting the same strain of HPV again.
Our immune system generally works by recognizing something that’s not right and building an immunity that means we can’t get the same infection again. But studies show our natural immunity against HPV isn’t very good so it can be possible to have the same infection again.
There’s still lots of research to be done to understand this properly and how reinfection could happen between partners.
Does my partner have it and how can I protect them?
There isn’t testing for HPV apart from as part of the national cervical screening program. Cervical screening is for anyone with a cervix aged between 25 and 64. This can include women, transgender men and people who are non-binary. Invitations to cervical screening start at 25 because in younger people, the changes to the cells in the cervix more often return to normal and are less likely to develop into cancer. Screening at a younger age would lead to unnecessary worry and treatment, and overall does more harm than good.
There are some ways to reduce the risk of getting or passing on HPV, but it’s important to remember it is a very common virus and it’s normal to have it at points in your life.
As HPV is passed between people during close skin to skin contact, barrier methods like condoms and dental dams can reduce risk, but they don’t work perfectly. Having HPV doesn’t mean you need to stop having sex with your partner but sexual health and consent is always important to talk about with any sexual partners.
But try not to worry about it too much. Even though HPV infection itself is common, it leading to cancer isn’t. Around 80% people will have an HPV infection at some point in their life but only a small percentage of people will develop a cancer linked to HPV.
There aren’t screening programs for all cancer types related to HPV as screening is only set up when there’s an effective test, and when saving lives can be balanced with not adding health risk. It’s important to remember that screening is for people without symptoms. If you are worried about a symptom or have noticed a change that is not normal for you or not going away, tell your doctor—whatever your age and regardless of whether you have been for screening recently or not.
Can I give HPV to my kids?
HPV can be passed between mother and child during pregnancy or delivery, but it’s not very likely. And if it does happen, usually the infection clears up by itself and there are no issues for the child.
There is more research needed to understand the transmission between mother and child. HPV can also be passed through breast feeding but this is very rare and shouldn’t be a reason not to breastfeed. If it’s something you are concerned about—talk to your doctor or midwife.
Should I get the HPV vaccine?
HPV vaccination is an important part of reducing the number of people with high risk HPV and in turn, the number of people who develop HPV related cancers. In the UK, all children between 11 and 13 are offered the HPV vaccine.
Vaccines work by reducing the risk of getting an infection, they’re not designed to get rid of an infection that is already there. The vaccine program includes children of this age as it is likely to be before any exposure to HPV which makes it work better. Once a person has been exposed to HPV, the vaccine becomes less effective.
You can request a vaccine for free up to the age for 25 if you didn’t have one when you were offered it at school. The vaccine is also available to men who have sex with men up to 45 through sexual health clinics. You can pay to have the vaccine privately if don’t meet these criteria, but the vaccine may not be effective if you’ve already been exposed to the virus, which most of us have been when we’re adults.
The best way to protect yourself against cervical cancer is to attend your regular cervical screening. The vaccine isn’t 100% effective at protecting against HPV so cervical screening is still important whether you have had the HPV vaccine or not.
Though sometimes some of the science is complicated, what having HPV means shouldn’t be—it’s normal! It’s hard to just ‘not worry,” but there’s not much you can do about your HPV status and having regular cervical screening is a really effective way of preventing cervical cancer.
Source: Read Full Article
