Scientists at St. Jude Children’s Research Hospital have solved an immunology puzzle. A CD8+ T cell can have two functionally distinct daughter cells after it divides, despite the cells being genetically identical. The researchers have explained how, revealing one method the immune system uses to provide immediate and long-term protection. The research appears today in Molecular Cell.
The researchers showed how a specific protein complex guides translation of an important immune transcription factor in one region of the parent T cell. When the cell divides, because the transcription factor is only in one region, it is then inherited asymmetrically into two daughter cells. The transcription factor drives expression of a set of genes in one daughter cell, pushing it to become an effector cell, while the other becomes a memory cell.
“Our results hint that events that happen very early in a T cell’s life can influence the function of the cell much later,” said corresponding author Doug Green, Ph.D., St. Jude Department of Immunology chair. “We have uncovered one way in which the immune system ensures that when T cells are activated, the response will be diverse, with some cells, the effectors, launching a rapid assault on the invader and others hanging back in reserve for later, as memory cells.”
Two very different daughters with the same DNA
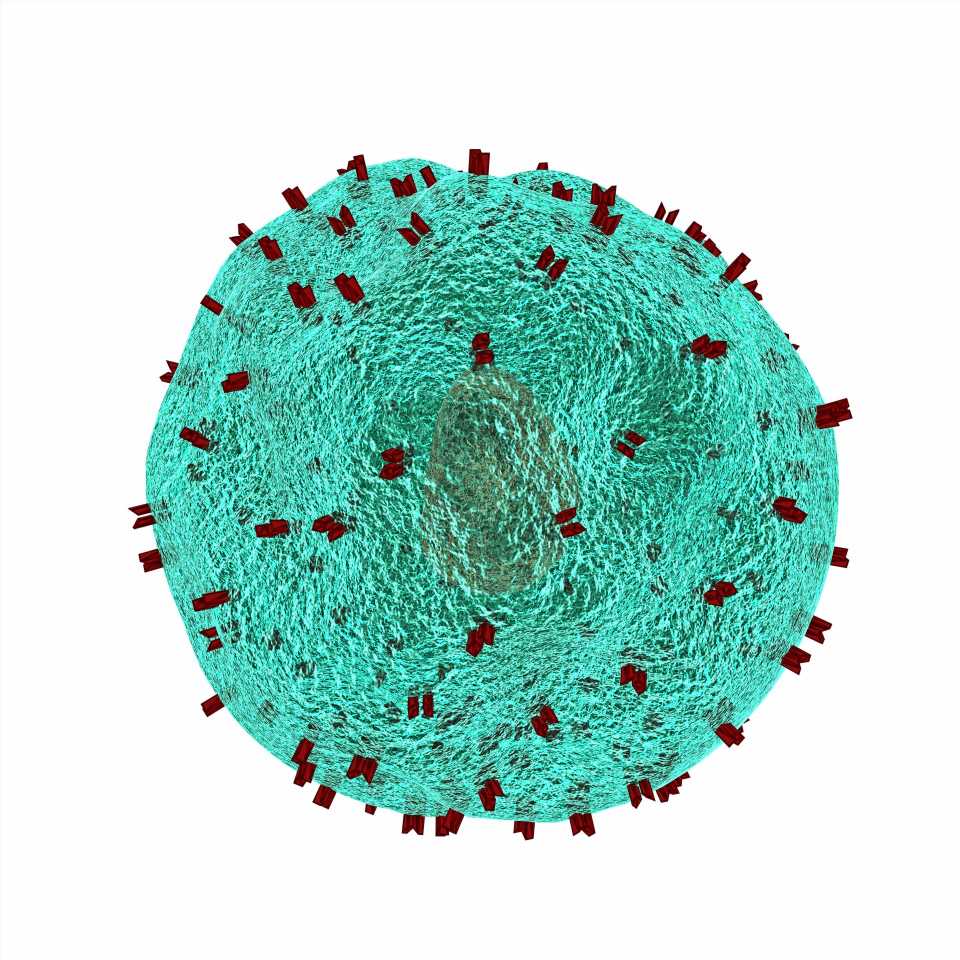
The immune system has many different cell types with varied functions. One major cell type is CD8+ T cells. These cells are responsible for directly killing infected and tumor cells. They are activated by a special cell that presents a bit of virus or tumor cell, called an antigen, on their surface. The point of contact between T cells and the antigen-presenting cells is called the immune synapse. After activation, the T cells divide into genetically identical daughter cells.
Many of the daughter cells become effector cells that also kill infected or cancer cells. However, some of the daughter cells become memory cells to help protect against future infections or the same cancer. Before this study, it was unclear how both effector and memory cells could come from the same parent T cell.
An unstable protein, lost without translation
As a first clue, Green’s group had previously shown that the first two daughter cells from an activated T-cell parent have different levels of the protein c-Myc. This is important, as c-Myc is a transcription factor known to drive expression of genes that make T cells become effector cells. However, c-Myc is unstable, half of all c-Myc in the cell disappears within 20 minutes. So how then is c-Myc present long enough and in the right position to be preferentially divided into one daughter cell?
Normally, the answer involves mRNA. mRNA serves as a template that cells use to make a protein. When an unstable protein is concentrated in one part of a cell, it is because its mRNA template is restricted to that location. However, c-myc mRNA transcripts appeared to be evenly distributed throughout the cell.
Instead, the researchers discovered that the protein complex that makes c-Myc was only present near the immune synapse. The specific complex responsible for translating c-Myc is called the eukaryotic translation initiation factor 4F (eIF4F) complex. The eIF4F complex is translation machinery, which takes mRNA messages and makes them into proteins, in this case, c-Myc.
The c-myc mRNA has a complicated structure on one end. Only the eIF4F complex can use the complicated structure of the c-myc mRNA to start the translation process into protein. Therefore, c-Myc is only produced where eIF4F is present, which relegates c-Myc to one side of the cell.
This is the first time that the location of translation machinery has been described as the reason why a protein is present in only one part of the cell.
Finding a molecular platform
While the location of eIF4F explains why c-Myc is only in one part of the cell, it revealed a new mystery: How did eIF4F become concentrated on one end of the cell?
The scientists used a special microscopy technique, called expansion microscopy, to “blow up” a T cell to learn how eIF4F moved through the cell. This is roughly the equivalent of blowing up a mouse to the size of an elephant. This study is the first time the technique was used with a primary T cell. Green’s group saw how eIF4F moved through the cell to one end by the immune synapse, including both trafficking mechanisms and eIF4F’s eventual placement on a molecular “platform” associated with the synapse.
Genetic ‘bar coding’ confirms the fate of sister cells
Green’s group verified that pairs of “sister” cells—daughter cells from the same parent—started expressing genes from the two different lineages, effector or memory. The group adopted a genetic “bar code” system to trace which individual cells were directly related. This was an extreme technical feat, as outside of the rearranged bar code sequence, there were many cells that were genetically identical. But the group was able to sequence the mRNA transcripts of these cells. The transcripts showed genetically identical sister cells with matching barcodes expressed different genes known to be related to their respective T-cell subtype.
Source: Read Full Article