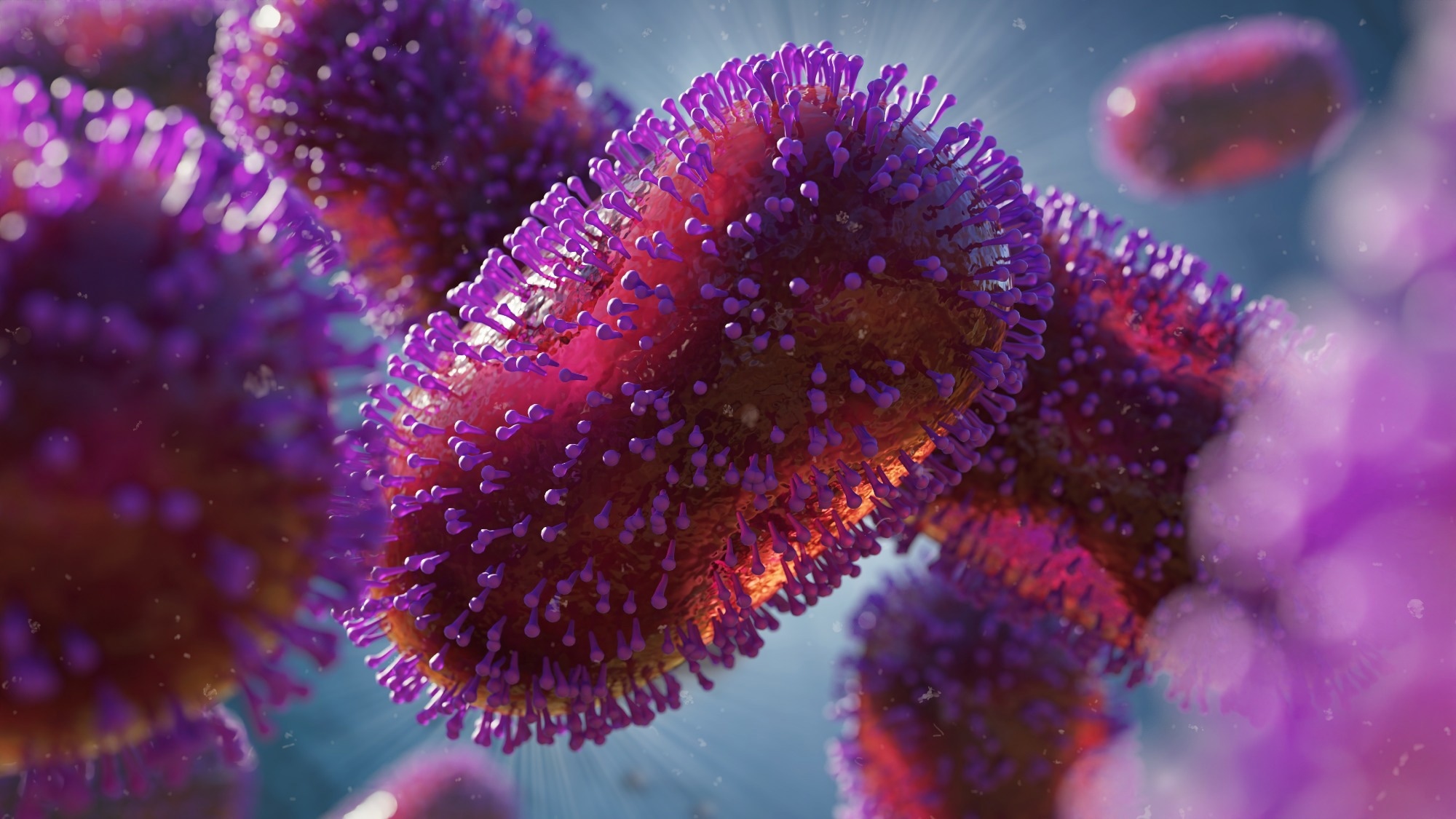
Studies have reported more than 60,000 human cases of monkeypox in non-endemic countries as of May 2022. The current outbreak has been observed to be different from the previous monkeypox infections in central and west Africa. This was due to the asynchronous evolution of lesions as well as more common perianal and genital localizations. This unusual outbreak of the monkeypox virus led the scientific community to discuss vaccination strategies for the high-risk groups, which mostly comprised men who have sex with men.
Background
Lab Diagnostics & Automation eBook

The smallpox vaccine has been reported to be 85% cross-protective against the monkeypox virus. However, its limitations include restriction to people aged 40 years and above and debatable background immunity. The unavailability of protective immunity among young people may lead to the circulation of the monkeypox virus among humans.
Previous experiments in animal models suggest that all the immune players help in viral clearance, with CD8+ T cells being the most important. Moreover, one study reported that all convalescent cases were positive for orthopoxvirus-specific IgG, IgM, B cell, and T cell responses. Also, an orthopoxvirus-specific immune response was observed in some people who did not develop monkeypox infection.
Smallpox vaccination was observed to be unable to provide complete protection against the monkeypox virus but could protect against severe disease. Furthermore, overproduction of cytokines has been observed in patients with severe monkeypox infection, suggesting a link between clinical severity and an unbalanced immune response. However, no information regarding the dynamics of immune response in humans in the current outbreak is available.
A new study published in The Lancet Infectious Diseases aimed to analyze the kinetics of the pox-specific T-cell induction, the inflammatory profile, and the inflammatory profile in human cases of the current monkeypox outbreak.
About the study
The study involved 17 patients with a laboratory-confirmed monkeypox virus positivity tested 10 to 12 days post the onset of symptoms and ten healthy controls. Samples collected from all the patients were divided into four groups: T0–T3, T4–T7, T8–T11, and T12–T20 days from the onset of symptoms. Demographic, epidemiological, laboratory, and clinical data were collected from all the patients.
Flow cytometry was done to analyze the activation and differentiation of CD4+ and CD8+ T-cells. Standard interferon-γ ELISpot was used to determine the frequency of T cell response to peptides from modified vaccinia virus Ankara (MVA). Assessment of spontaneous cytokine production was carried out through incubation of peripheral blood mononuclear cells (PBMCs) collected from all participants in DMSO. ELISA assay was carried out to evaluate the production of cytokines after specific stimulation. Finally, quantifying IL-1β, IL-6, IL-8, and TNF in the plasma of patients was done using automated multiplex immunoassays.
Study findings
The results indicated the median age of the patients to be 39.5 years. 7 were reported to be HIV-positive with antiretroviral therapy but undetectable HIV-RNA and a CD4+ T-cell count greater than 350 cells/µl. The 10 HIV-negative participants were reported to be on pre-exposure prophylaxis (PrEP). The transmission route was reported to be sexual intercourse for 14 patients.
Systemic symptoms were observed in 14 patients, while those without systemic symptoms were considered paucisymptomatic. One patient had received a smallpox vaccination during childhood, while five were treated with antiviral drugs. The median recovery time was reported to be 15 days.
A lower percentage of CD4+ T-cells and a higher percentage of CD8+ T-cells were reported in patients early after infection compared to healthy controls. Six out of nine monkeypox cases were reported to have a lower naive CD4+ T cell frequency than healthy controls. A lower proportion of naive and higher terminally differentiated CD8+ T cells was observed in all patients. However, the proportion of CD4+ effector memory T cells frequency was observed to be similar in patients and healthy controls after 12 to 20 days.
A higher CD4+CD38+ and CD8+CD38+ T-cells frequency was observed in patients compared to healthy controls, which were also similar for PD-1 and CD57 markers. No immune cell profile differences were observed between HIV-positive and HIV-negative patients while a less altered immune profile was observed for paucisymptomatic patients. Higher inflammatory cytokines (IL-1β, IL-6, IL-8, and TNF) were observed in patients with monkeypox virus as compared to controls which remained higher even after recovery.
Furthermore, higher expression of CCR7, CD69, CXCR5, CD95, CCR6, CXCR3, CD28, CD4RA, and CD27 was observed in patients as compared to healthy controls in the post-acute phase. Similar results were observed for CD8+ T cells along with the re-expression of CD45RA. Additionally, patients with monkeypox showed a higher percentage of effector memory T cells re-expressing CD45RA that expressed CD57, PD1, or both.
Therefore, the current study demonstrated an early expansion of activated effector CD4+ and CD8+ T cells as a result of monkeypox virus infection which persists over time. All participants also developed a strong cytokine response irrespective of HIV infection. Thus, the MVA vaccine can be used as an anti-monkeypox vaccine for the high-risk population. Further research on prolonged immunity is required to support the current hypothesis.
Limitations
The study has certain limitations. First, data on humoral response analysis was not available. Second, only three poxvirus proteins were used as antigens. Third, the study does not involve a randomized selection of participants. Fourth, the number of participants was limited.
- Agrati, C. et al. (2022). Immunological signature in human cases of monkeypox infection in 2022 outbreak: an observational study. The Lancet Infectious Diseases. doi: https://doi.org/10.1016/S1473-3099(22)00662-4. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(22)00662-4/fulltext.
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antiretroviral, Assay, B Cell, Blood, CD4, Cell, Cytokine, Cytokines, Cytometry, Drugs, ELISA, Evolution, Flow Cytometry, Frequency, HIV, Immune Response, immunity, Immunoassays, Infectious Diseases, Interferon, Laboratory, Monkeypox, Peptides, Pre-Exposure Prophylaxis, Prophylaxis, Research, RNA, Smallpox, T-Cell, Vaccine, Vaccinia Virus, Virus

Written by
Suchandrima Bhowmik
Suchandrima has a Bachelor of Science (B.Sc.) degree in Microbiology and a Master of Science (M.Sc.) degree in Microbiology from the University of Calcutta, India. The study of health and diseases was always very important to her. In addition to Microbiology, she also gained extensive knowledge in Biochemistry, Immunology, Medical Microbiology, Metabolism, and Biotechnology as part of her master's degree.
Source: Read Full Article
