Although rare, mucosal melanoma in humans has a low survival rate. It has been difficult to investigate due to a lack of similar cancers in animals for study.
Researchers explored a protein common to human and canine mucosal melanoma. The protein seems to be what makes this cancer so problematic, as it mobilizes the cancer cells, allowing them to spread. Researchers hope that eliminating this protein could lead to a potential treatment. The study is published in Molecular Cancer Research.
Melanoma is a type of cancer that begins in the melanocytes, the pigments that give skin its range of tones. Skin cancer accounts for about 90% of all melanomas in humans, but a small percentage are mucosal melanomas, which can manifest in the body’s various mucosal linings such as in the nose. Mucosal melanomas are hard to detect and even harder to treat, with a five-year survival rate of only 25%. Partly due to its rarity, and partly due to the lack of analogous forms of cancer in animals, it has been very difficult to research mucosal melanoma.
But a team of researchers, including those from the University of Tokyo’s Laboratory of Veterinary Surgery, has studied a common form of cancer in dogs and found some specific biological similarities that mean two things. Firstly, that there is a suitable animal model for mucosal melanoma in humans, and secondly, that they both involve a very specific marker that could be a target for reducing the spread of this, and potentially other, cancers.
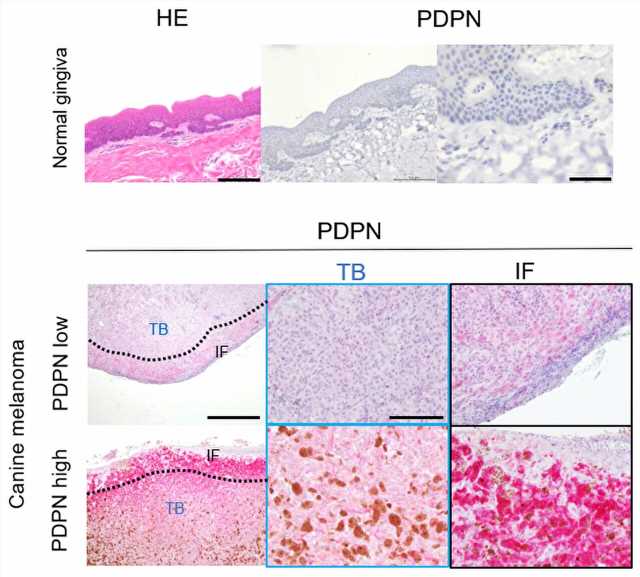
“Even though mucosal melanoma is not so common in humans, it is very common in dogs. There was no known connection between the two, but we have recently discovered something common to both,” said Assistant Professor Daiki Kato. “There is a protein that accompanies mucosal melanomas called podoplanin (PDPN). It’s a membrane protein, meaning it is involved in some functions on the surface of a cell. We found that patients suffering mucosal melanoma with a high presence of PDPN succumbed to their cancer much sooner than those with less.”
-
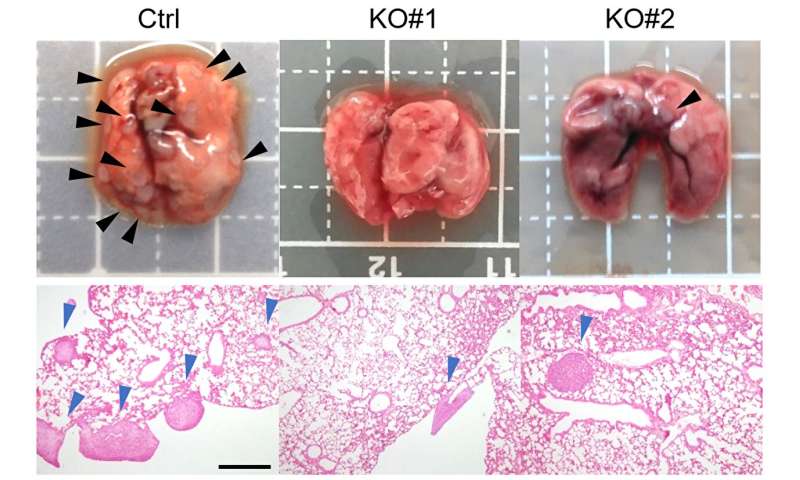
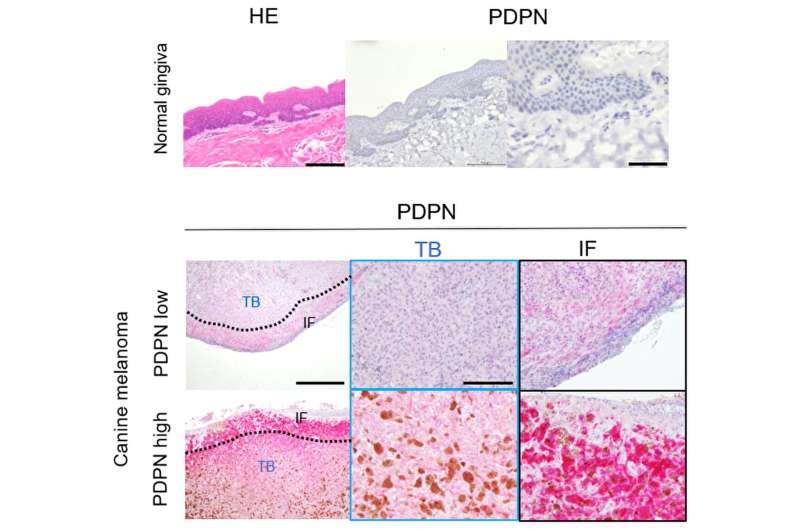
Photographs and microscope images of tissue containing a tumor. The sample on the left is the control sample, and the other two had reduced PDPN and show reduced metastatic sites. Credit: ©2023 Kato et al. CC-BY
-
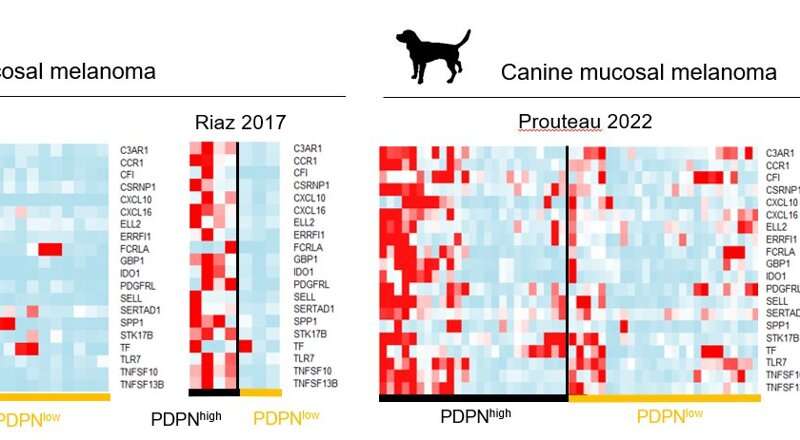
A heat map to show the dramatic similarity of expression of genes regulated by PDPN in both human and canine mucosal melanoma. Credit: ©2023 Kato et al. CC-BY
The team studied PDPN to see what might make it so potentially deadly. It seems the protein can metastasize, or mobilize, otherwise static tumor cells. PDPN morphs tumor cells into something resembling a free-moving amoeba, which can squeeze between gaps in healthy tissue and move around to settle elsewhere in the body. This mechanism would explain why mucosal melanoma, in particular, sees such a quick spread of the cancer throughout the body.
“We are sure that this happens, but we still do not understand the entire mechanism behind why,” said Kato.
“A big challenge is actually our data. As mucosal melanoma is rare, there just isn’t a lot of human data to learn from; our study had to combine different data sets and is not as complete as we would like. However, our tests involving PDPN do confirm our suspicion. When we took mucosal melanoma samples from dogs and eliminated the PDPN, the resulting tumor released far fewer metastasized cells which could spread and cause more harm. Though the samples came from dogs, that part of the experiment was carried out in mice.”
This means PDPN could be a target for antibody therapy. If new drugs can eliminate PDPN in patients with mucosal melanoma, it might reduce the spread, and suffering, it causes. The team is working toward this now and aims to run clinical trials in dogs, within a few years.
“Of course, we will continue to work toward treatments for both canine and human cancers. PDPN is just one avenue of attack,” said Kato. “But also of great importance is the fact that we have found an animal model for an often fatal human cancer, which opens up many possibilities for study.”
More information:
Podoplanin drives amoeboid invasion in canine and human mucosal melanoma, Molecular Cancer Research (2023). DOI: 10.1158/1541-7786.MCR-22-0929
Journal information:
Molecular Cancer Research
Source: Read Full Article