Being overweight impacts your heart health in more ways than you might think. A new Journal of the American College of Cardiology review paper from Mayo Clinic outlines how obesity affects the common tests used to diagnose heart disease and impacts treatments. Cardiovascular disease is the leading cause of death in the U.S. and globally, yet it is largely preventable.
“Excess fat acts as a kind of filter and can skew test readings to under-or overdiagnosis,” says senior author Francisco Lopez-Jimenez, M.D., director of preventive cardiology at Mayo Clinic. “Obesity affects nearly all the diagnostic tests used in cardiology, such as ECG, CT scan, MRI and echocardiogram.”
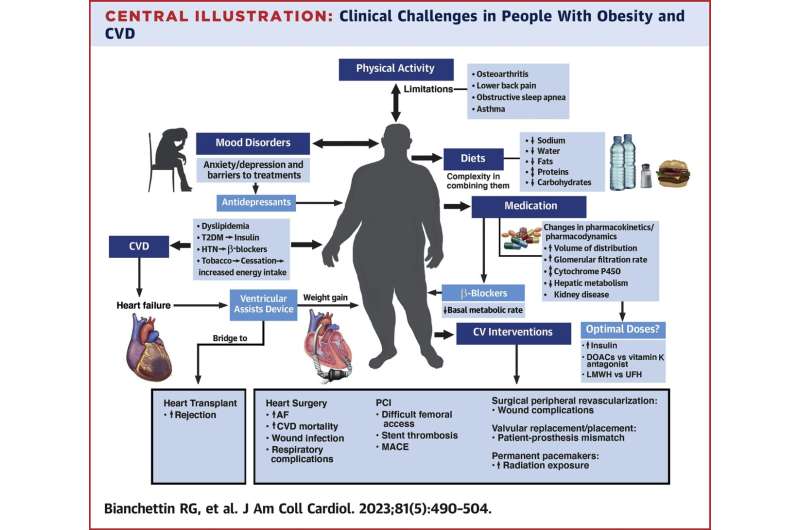
Procedural interventions such as stent placement via the leg, or heart surgery, can be more difficult to perform in patients with significant obesity and may involve more complications, like increased risk of infection at the wound site.
Common drug therapies to treat cardiovascular disease may need to be adjusted up or down in patients with obesity. Some medications, such as beta-blockers, may affect a patient’s ability to lose weight, and Dr. Lopez-Jimenez stresses the importance of trying alternative approaches to prevent these patients from gaining weight or help them to lose weight.
Recommendations to lose weight can be difficult to follow because heart patients have a harder time moving and will feel symptoms like shortness of breath when they exercise. Those symptoms often discourage patients from doing physical activity, but Dr. Lopez-Jimenez notes that exercise is important, not only to lose weight but for heart health.
“Obesity is an important risk factor to address in patients with heart disease and it requires us to do something,” says Dr. Lopez-Jimenez.” The patient needs to know that their clinician can help them lose weight. Overall, weight loss solutions come down to finding the right therapy for the patient.”
A standard weight loss program will involve a therapist, dietitian and sometimes a psychologist. If that doesn’t do enough, Dr. Lopez-Jimenez says there are other resources like bariatric surgery and medications that can effectively help patients lose weight. Mayo Clinic recently started a multidisciplinary cardiometabolic program to address obesity, reduce related disease conditions and help patients improve their quality of life.
Accurately defining a person’s level of obesity is important. Body mass index (BMI)―a measure of body fat based on height and weight―has long been used to define the severity of obesity. But people with significant amounts of muscle will have a high BMI. People with little muscle mass and more waistline fat might record a low BMI but have normal-weight obesity. Measurements such as waist-to-hip ratio and waist circumference provide a more accurate assessment of cardiovascular risk.
“In general, patients with heart disease and a particularly advanced degree of obesity will benefit from trying lifestyle modification. And if that doesn’t work, or if they have tried that in the past, it is reasonable to consider bariatric surgery or medications,” says Dr. Lopez-Jimenez.
More information:
Rosana G. Bianchettin et al, Challenges in Cardiovascular Evaluation and Management of Obese Patients, Journal of the American College of Cardiology (2023). DOI: 10.1016/j.jacc.2022.11.031
Journal information:
Journal of the American College of Cardiology
Source: Read Full Article
