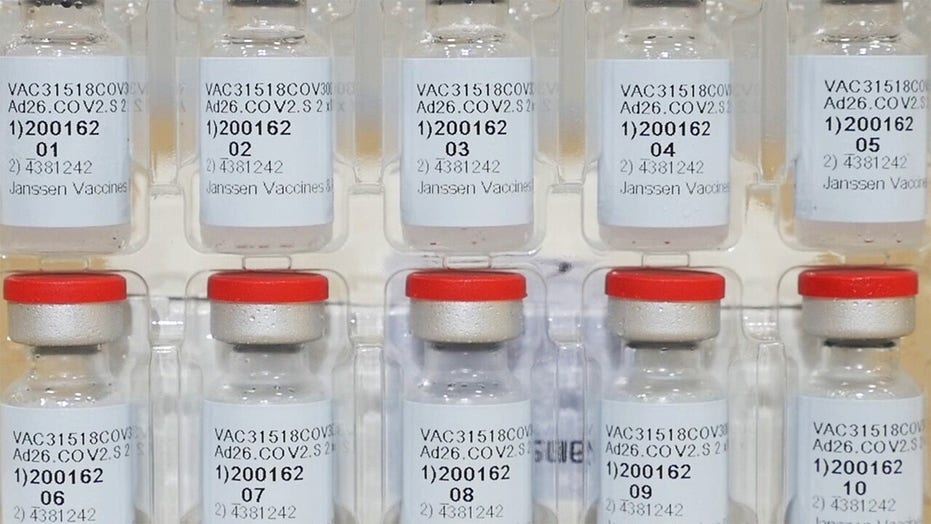
Feds recommend pause in Johnson & Johnson COVID-19 vaccine rollout
The CDC and FDA will pause the use of the Johnson & Johnson COVID-19 vaccine at federal sites after several instances of severe blood clots in recipients.
With Johnson & Johnson’s COVID-19 vaccine facing an FDA-recommended pause after several instances of severe blood clots were reported in recipients, those who had scheduled J&J shots could see a bumpy rescheduling process involving canceled or delayed appointments, or even find themselves lined up to receive an alternative vaccine if supply allows.
For those facing the latter, it’s important to know how the shots compare.
Vaccines developed by Moderna and Pfizer-BioNTech operate on a newer platform with mRNA, or messenger RNA, technology, while Johnson & Johnson’s candidate involves a more traditional modified adenovirus vector vaccine with a durable protein exterior encasing the DNA, lending itself to a longer shelf-life.
Clinical trials indicated vaccines developed by Pfizer and Moderna were about 95% effective against symptomatic illness, and Johnson & Johnson’s candidate had a 66.3% efficacy. Trial data also revealed all three vaccines were highly effective in preventing hospitalizations and deaths.
WHAT’S THE DIFFERENCE BETWEEN MRNA VACCINES AND CONVENTIONAL ONES?
While the Pfizer and Moderna COVID-19 vaccines train the body to recognize the spike protein that coats the outer surface of the coronavirus, the J&J and AstraZeneca vaccines use a cold virus, called an adenovirus, to carry the spike gene into the body. J&J uses a human adenovirus to create its vaccine while AstraZeneca uses a chimpanzee version. The AstraZeneca vaccine is not yet authorized for use in the U.S.
It’s also important to note that Pfizer and Moderna’s vaccines each require a two-dose regimen while, Johnson & Johnson’s product requires just a single dose, which eased logistics prior to the national pause Tuesday. Dr. Peter Marks, director at FDA Center for Biologics Evaluation and Research, told reporters on Tuesday a probable cause behind the clotting that occurred among vaccine recipients might include a similar mechanism seen with AstraZeneca’s product, another adenoviral vector vaccine being rolled out in Europe, in which a rare immune response occurred post-vaccination, leading to activation of platelets and “extremely rare” blood clots.
According to the FDA, there have been six reported cases of the rare and severe type of blood clot in over 6.8 million Johnson & Johnson COVID-19 vaccine recipients. The FDA said Tuesday it expects the pause to last several days as experts review available data.
Johnson & Johnson’s vaccine candidate is stable for up to two years at -20 degrees Celsius and at least three months at 2 to 8 degrees Celsius. Moderna’s vaccine can last at -20 degrees Celsius for six months and 2 to 8 degrees Celsius for 30 days. Meanwhile, in February the FDA eased permitted shipping and two-week storage temperatures for the Pfizer vaccine to -25 degrees Celsius to -15 degrees Celsius in a significant shift from an ultra-cold temperature requirement of -80 degrees Celsius and -60 degrees Celsius for up to six months.
Pfizer’s vaccine was authorized for use in people 16 years and older, while Moderna and J&J’s was approved for those 18 and up. Pfizer announced last week that it submitted a request for emergency use authorization to begin administering its COVID-19 vaccine to adolescents between the ages of 12 and 15 in the U.S.
Fox News’ Alexandria Hein and the Associated Press contributed to this report.
Source: Read Full Article
