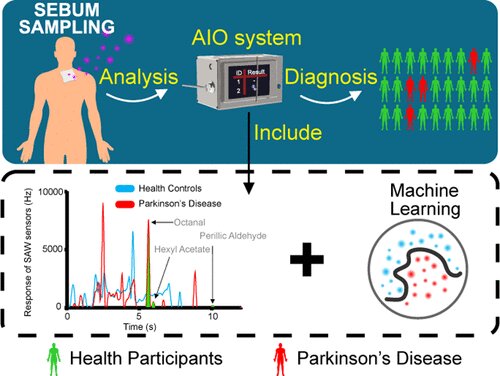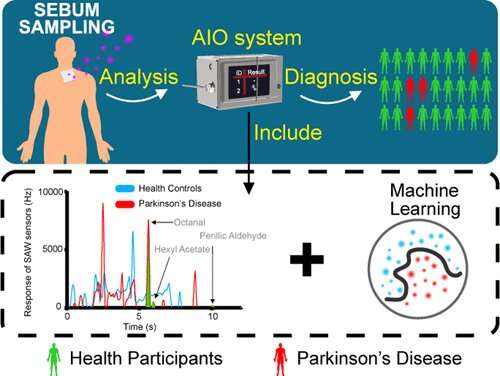
A couple of years ago, a woman named Joy Milne made headlines when scientists discovered that she could “smell” Parkinson’s disease (PD) on people with the neurodegenerative disorder. Since then, researchers have been trying to build devices that could diagnose PD through odor compounds on the skin. Now, researchers reporting in ACS Omega have developed a portable, artificially intelligent olfactory system, or “e-nose,” that could someday diagnose the disease in a doctor’s office.
PD causes motor symptoms, such as tremors, rigidity and trouble walking, as well as non-motor symptoms, including depression and dementia. Although there’s no cure, early diagnosis and treatment can improve one’s quality of life, relieve symptoms and prolong survival. However, the disease usually isn’t identified until patients develop motor symptoms, and by that time, they’ve already experienced irreversible neuron loss. Recently, scientists discovered that people with PD secrete increased sebum (an oily, waxy substance produced by the skin’s sebaceous glands), along with increased production of yeast, enzymes and hormones, which combine to produce certain odors. Although human “super smellers” like Milne are very rare, researchers have used gas chromatography (GC)-mass spectrometry to analyze odor compounds in the sebum of people with PD. But the instruments are bulky, slow and expensive. Jun Liu, Xing Chen and colleagues wanted to develop a fast, easy to use, portable and inexpensive GC system to diagnose PD through smell, making it suitable for point-of-care testing.
The researchers developed an e-nose, combining GC with a surface acoustic wave sensor—which measures gaseous compounds through their interaction with a sound wave—and machine learning algorithms. The team collected sebum samples from 31 PD patients and 32 healthy controls by swabbing their upper backs with gauze. They analyzed volatile organic compounds emanating from the gauze with the e-nose, finding three odor compounds (octanal, hexyl acetate and perillic aldehyde) that were significantly different between the two groups, which they used to build a model for PD diagnosis.
Source: Read Full Article