
The emergence of SARS-CoV-2 (the virus that causes COVID) has changed the world as we know it. Although new vaccines and antiviral treatments have brought hope, the pesky virus has continued to mutate and evade us.
Knowledge has been building about how this virus operates and why it continues to pose a challenge. We have heard reports of the virus resulting in “immune exhaustion”, potentially triggering autoimmunity (when the body attacks itself) and even shrinking the brain.
Now scientists are discovering just how the virus impacts DNA. It looks like this could give it the power to evade our immune system—but that doesn’t mean it can get passed on genetically.
So very, very sneaky
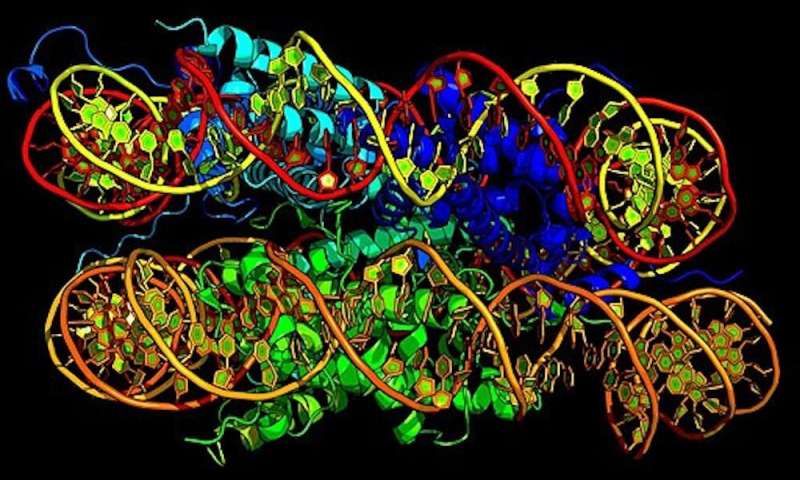
Research published in Nature earlier this month found one of the SARS-CoV-2 proteins is able to imitate one of our cellular proteins called histones.
Histones are required to condense DNA. This allows DNA to be packaged into tight bundles, ensuring it all fits within a cell. Histones frequently change and respond to external cues to regulate the DNA. They help to switch genes on or off.
The new finding indicates SARS-CoV-2 can disrupt our genes and their expression.
So what does the study show?
The study found one of the SARS-CoV-2 proteins—called “open reading frame 8” (ORF8) protein—has evolved to mimic a part of human histone called H3.
This mimicking seems to alter the way H3 functions and changes the host’s epigenetics. The researchers found that when they deleted a critical region of the ORF8 protein or the entire ORF8 protein, the virus was not able to replicate to the same high levels as the original COVID strain in human lung alveolar cells. This suggests the ORF8 protein contributes to COVID disease severity.
The research reveals an epigenetic mechanism that promotes SARS-CoV-2 virulence within the population. These findings may also help researchers understand how COVID develops and the disease severity of emerging viral strains.
What are ‘epigenetics’ again?
Our genes can be thought of as a blueprint that determines how our bodies are built. Collectively, the study of our genes and how these are passed from parent to offspring is called “genetics”.
“Epigenetics” refers to the factors that influence which genes are switched on or off. These factors include lifestyle elements we can control (think diet, exercise, sleep, smoking), age or even some infections.
So, whereas genetics refers to the blueprint (genes), epigenetics refers to how that blueprint is read (gene expression).
Some epigentic factors can be passed on from parent to child, but this does not mean the newly reported impact of SARS-CoV-2 on our histones will be.
So, does this change what we already knew?
This is not the first time research has found that pathogen (invading bugs or diseases) affect our epigenetics.
It is well established that the pathogen that causes tuberculosis, Mycobacterium tuberculosis, changes the host gene expression through histone modification to promote its own survival.
Similarly, viruses like adenovirus (which can cause colds, conjunctivitis, gastro and more), human papilloma virus and herpes viruses are all known to alter host epigenetics through various mechanisms.
Evidence has been growing to suggest COVID impacts our immunity, but questions still remain as to how. This newly discovered SARS-CoV-2 mechanism provides another piece of the puzzle and might help to explain one way that the virus disrupts epigenetics to lead to more severe COVID.
Another reason not to get COVID
Epigenetics is a relatively new field of study that holds promise for the development of new therapies.
It is still early days for this research, but future investigation might look for ways to counteract the viruses impact on our histones as a way of protecting our immune system.
Source: Read Full Article
