Professor Maureen R. Hanson of the Department of Molecular Biology and Genetics, Cornell University, Ithaca, New York, has looked into historical outbreaks of myalgic encephalomyelitis (ME), also known as chronic fatigue syndrome (CFS), and their association with enteroviruses and other pathogens.
In a paper, “The viral origin of myalgic encephalomyelitis/chronic fatigue syndrome,” published in PLOS Pathogens, professor Hanson explores several hypotheses related to the causes of ME/CFS, including a likely culprit in viral infections, particularly those from the enterovirus family.
The exact causes of ME/CFS are not fully understood, and it is considered a complex and multifactorial condition. Several theories and factors have been proposed as potential contributors to ME/CFS, but no single cause has been definitively identified.
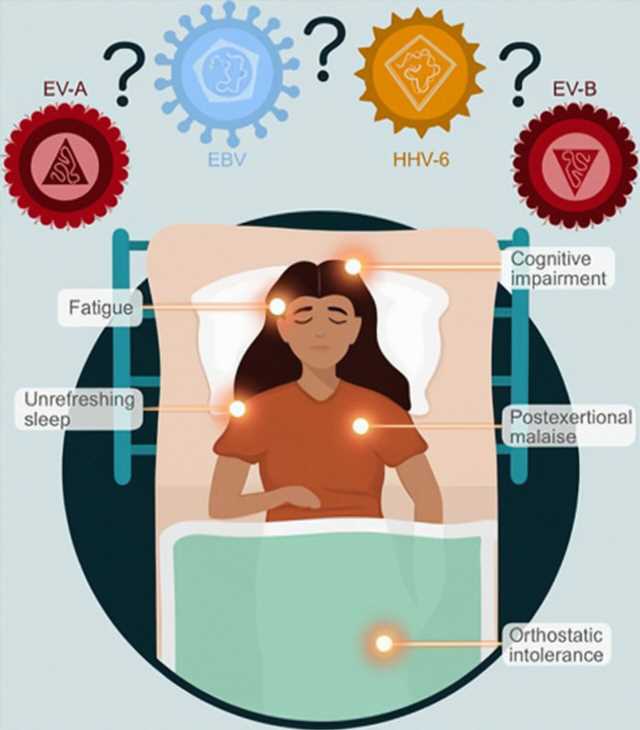
Hanson makes the case that some causes are more likely than others, including:
- Infections with the enterovirus family of viruses. This hypothesis is based on historical outbreaks of ME/CFS coinciding with outbreaks of diseases caused by enteroviruses, as well as evidence of chronic viral infection in some ME/CFS patients. While this could be causal to many more cases, identifying the specific virus that was infecting an individual who later acquired ME/CFS is not possible.
- Human herpesviruses (HHVs), such as Epstein-Barr virus and HHV-6. In ME/CFS, these are a potential source. Some ME/CFS patients report an acute infection with HHVs at the onset of their illness, and reactivation of these viruses may contribute to the condition.
- Post-viral syndromes, including post-acute sequelae of COVID-19 (PASC). These are included in an emerging area of clinical understanding. Some individuals with mild or asymptomatic COVID-19 later experience a post-viral illness that shares symptoms with ME/CFS. This raises questions about the relationship between other lesser-known or less apparent infections and their potential to cause post-viral syndromes and ME/CFS.
In the light of a major viral pandemic with lingering ME/CFS conditions, Hanson compiled information on historical ME/CFS outbreaks with studies on infections like Epstein-Barr virus, Q fever, Ross River virus, influenza and previous ME/CFS patient research, and interrogated varying criteria used by research groups and clinicians to define ME/CFS.
Focusing on viral infections is an intriguing investigative path, as there are already many conditions associated with ME/CFS, almost as if a researcher could pick anywhere to start pulling at the connecting threads of the condition.
There are immune system abnormalities linked to ME/CFS; genetic factors may play a role in susceptibility. The central nervous system has associations with many of the symptoms. A host of potential environmental factors, such as toxins, stress, and trauma may be implicated. Recent research indicates issues with cellular energy metabolism, particularly involving mitochondria, leading to the fatigue and reduced stamina. Hormonal dysregulation and/or gut microbiota could play a role, and the list goes on.
Hanson argues that there is no proof that multiple pathogens can cause ME/CFS. She suggests that the hypothesis persists due to the overinterpretation of data from previous studies where the initial infection type was either missed, inferred but not verified, or where the symptom survey did not include ME/CFS defining criteria.
Currently, there is no specific diagnostic test or universally effective treatment for ME/CFS, which makes it a challenging condition to manage. Treatment typically focuses on symptom management by attempting to improve the quality of life for individuals through traditional, good doctorly advice of “Exercise regularly, eat right, get plenty of sleep.” The condition can be frustrating for patients who follow such advice and yet find no relief.
Before the SARS-CoV-2 pandemic, the ability of RNA viruses to persist in tissues for long periods was largely ignored, according to Hanson. Recognizing that EVs are prime candidates for causing ME/CFS suggests the importance of pursuing a relevant inquiry into this diverse virus family.
The global laboratory
Sixty-five million long COVID sufferers worldwide have prompted the US government to devise PASC to describe a post-acute illness syndrome. Most relevant to ME/CFS is that some people who suffered mild or asymptomatic cases of COVID-19 later began experiencing a post-viral illness that fulfills most or even all of the criteria for ME/CFS.
Increasingly, these people are told by their doctors that they have ME/CFS, but the diagnostic criteria were created six years before SARS-CoV-2 emerged. Those who acquired ME/CFS before the SARS-CoV-2 outbreak also number in the tens of millions, and the source of their initial infection often remains a mystery.
Hanson suggests that the overlap in symptoms between some forms of post-COVID illness and ME/CFS suggests that disruptions in the same pathways may be occurring in both diseases, but to conclude that the two syndromes are identical without more data, especially at the molecular level, is currently unwarranted. Any SARS-specific antiviral treatments will not be effective for ME/CFS patients.
If it were not for COVID-19 hitting everywhere all at once, ME/CFS caused by SARS-CoV-2 might also be flying under the radar of the clinical and research communities. Now that the link between a viral infection and ME/CFS has been firmly detected, Hanson is urging an inquiry into the prime candidate for previously existing ME/CFS cases.
More information:
Maureen R. Hanson et al, The viral origin of myalgic encephalomyelitis/chronic fatigue syndrome, PLOS Pathogens (2023). DOI: 10.1371/journal.ppat.1011523
Journal information:
PLoS Pathogens
Source: Read Full Article