Almost 85,000 laboratory-confirmed monkeypox (Mpox) cases and 80 deaths have been reported between January 1, 2022, and January 15, 2023, to the World Health Organization (WHO) in 110 countries, areas, or territories in the six WHO regions. A total of 11 countries have reported an increase in the weekly number of cases between January 2-15, 2023, with the highest increase reported in Mexico. However, 78 of the 110 countries have not reported new cases for over 21 days.
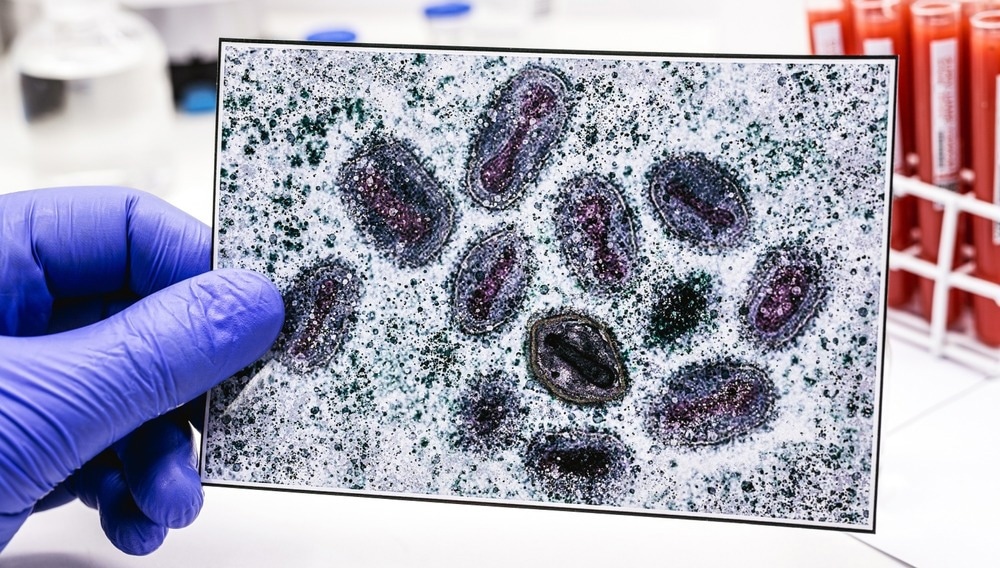
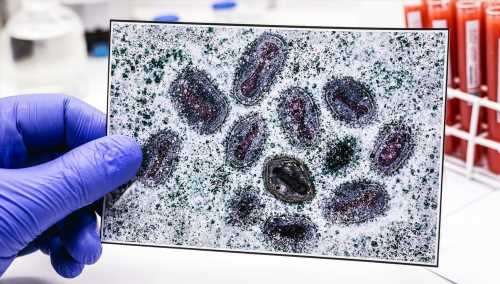
Study: External situation report #14- 19 January 2023. Image Credit: RHJPhotos / Shutterstock.com
Global Mpox cases
The number of new weekly Mpox cases decreased by 12.7% in week January 2 compared to week 1. The largest proportional reduction has been observed in the European Region and the Region of the Americas. Nevertheless, five deaths have been reported in the Americas region between January 2-15, 2023.
Ten countries reported the highest cumulative number of cases globally as of January 15, 2023, including Spain, Brazil, Germany, Canada, Mexico, Peru, the United Kingdom, Colombia, France, and the United States of America.
Most Mpox cases have been detected in men with a median age of 34. In addition, over 84% of Mpox cases have been identified among individuals who identified as bisexual, gay, and other men who have sex with men.
The two most common transmission routes appear to be through the skin and mucosal contact during sexual activities. The most common setting for Mpox exposure has been parties where sexual contact was involved. Rashes appear to be the most common symptom of Mpox infection, followed by fever and genital and systemic rash.
A new external situation report published by WHO discusses genomic sequencing of the Mpox virus and provides public and clinical health links between the human immunodeficiency virus (HIV) and Mpox.
Links between HIV and Mpox
Out of 44% of Mpox cases with information on HIV status, 48% were reported to live with HIV. Between 44-77% of individuals diagnosed with Mpox without a history of HIV were reported to access HIV services and use Anti-Retroviral Therapy (ART) for pre-exposure prophylaxis (PrEP) to prevent HIV.
Previous epidemiological data have indicated that people with poorly controlled HIV are at a higher risk of severe Mpox infections. Higher hospitalization rates for Mpox were observed among people living with HIV. The association between untreated HIV and Mpox severity emphasizes the need for achieving viral suppression, understanding the status of HIV, and accessing anti-retroviral treatment.
Transmission of Mpox among men who identify as gay or bisexual, sex workers, and transgender people has led to significant stigma and discrimination in healthcare settings, which could hinder HIV control and suppress the Mpox outbreak response.
The emergency response to Mpox in many countries that reported their first Mpox cases in 2022 utilized links between HIV services and communities at risk for Mpox. This helped in the implementation of interventions for the diagnosis, treatment, and prevention of Mpox in HIV services.
Genetics & Genomics eBook

Moreover, the WHO is working to establish recommendations for a long-term approach to integrate interventions to control Mpox transmission, especially for high-risk communities.
Laboratory responses
Laboratory testing is essential for the surveillance of disease, understanding local and global transmission, and managing cases. The WHO has supported the development and evaluation of numerous diagnostic kits for detecting the Mpox virus. The WHO collaborated with the Robert Koch Institute to evaluate 11 commercial PCR assays for the detection of MPXV DNA. As a result, 90,000 commercial molecular tests have been procured by WHO for over 60 countries across five WHO regions. This collaboration also helped in the exchange of reagents between laboratories across the world.
The WHO has provided a shipping fund for the shipment of samples to international referral laboratories for confirmatory testing in the case of countries with limited access to molecular diagnostics. Furthermore, the WHO has developed two target product profiles (TPPs) for MPXV diagnostics where TPP1 involves tests to be used for Mpox diagnosis within health care settings and laboratories, with TPP2 involving tests as aids for the diagnosis of Mpox.
Molecular epidemiology of the Mpox virus
The WHO developed new nomenclatures for Mpox clades. The two Mpox clades are known as clades I and II, previously referred to as the Congo basin (or Central African) clade and the West African clade, respectively.
Clade II comprises subclades IIa and IIb and causes less severe disease as compared to clade I. The ongoing outbreak is due to clade IIb and is divided into many more lineages and sublineages. Phylogenetic analysis of this clade has reported many more mutations than expected from Mpox.
The mutation rate from 2017 is about 20-fold greater as compared to the long-term evolutionary rate, with a high prevalence of a specific mutation pattern (cytosine deamination by molecules in the APOBEC3 family). No such sequence has been observed before 2017, thus suggesting that the current epidemic arose from an animal-to-human jump that took place before 2017.
Most of the clade IIb sequences from 2022 have been reported to belong to the clade IIb.B.1 lineage. However, the animal reservoir of Mpox remains unclear. Clade I and IIa sequences have been detected in animal hosts, while clade IIb has only been detected in humans.
Mpox in the African region
Over 1,200 laboratory-confirmed cases have been reported from 10 countries in the WHO African Region between January 1, 2022, and January 15, 2023. Two of these countries had never reported a human Mpox case before 2022.
Six countries with the highest number of cases in the African region include Liberia, the Central African Republic (CAR), Cameroon, Ghana, the Democratic Republic of the Congo (DRC), and Nigeria. The average age of people with Mpox between January and December 2022 has been reported to be 21 years, with a majority of patients being men.
Sixteen deaths have been reported due to Mpox in Ghana, Nigeria, Sudan, Mozambique, and Cameroon. The most common symptoms include rash, pain, fever, dysphagia, and headache.
The WHO Regional Office for Africa (AFRO) is providing support to countries to determine modes of transmission and the characteristics of Mpox cases in the region. AFRO is also helping improve laboratory testing capacities and the performance of genomic sequencing to identify the main clades of the current outbreak. However, both clades are currently circulating in Africa and leading to disease.
A risk communication and community engagement (RCCE) plan and strategy are being developed to further help control the current Mpox outbreak.
- Multi-country outbreak of mpox. External situation report #14- 19 January 2023. Available from: https://www.who.int/publications/m/item/multi-country-outbreak-of-mpox–external-situation-report-14–19-january-2023.
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: AIDS, Antiretroviral, Cytosine, Diagnostic, Diagnostics, DNA, Dysphagia, Epidemiology, Fever, Genomic, Genomic Sequencing, Headache, Health Care, Healthcare, HIV, Immunodeficiency, Laboratory, Molecular Diagnostics, Monkeypox, Mutation, Pain, Pre-Exposure Prophylaxis, Prophylaxis, Rash, Reagents, Skin, Virus

Written by
Suchandrima Bhowmik
Suchandrima has a Bachelor of Science (B.Sc.) degree in Microbiology and a Master of Science (M.Sc.) degree in Microbiology from the University of Calcutta, India. The study of health and diseases was always very important to her. In addition to Microbiology, she also gained extensive knowledge in Biochemistry, Immunology, Medical Microbiology, Metabolism, and Biotechnology as part of her master's degree.
Source: Read Full Article