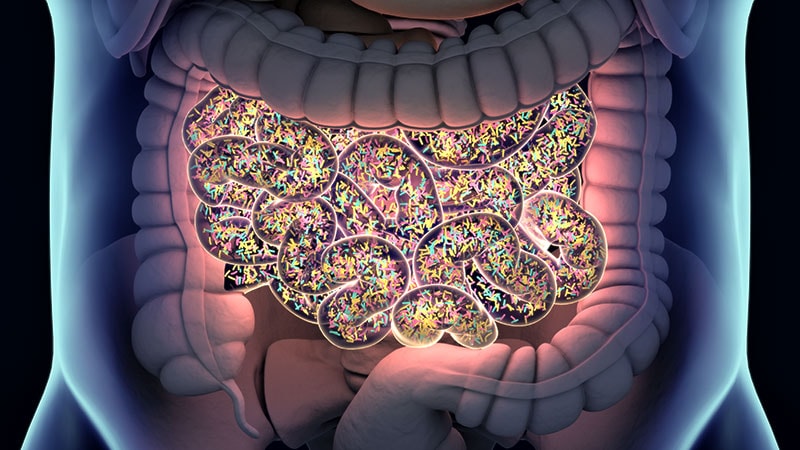
HONOLULU — What we eat and what’s in the gut may influence lung health for better or worse, suggest new data from an ongoing study of lung function in New York City firefighters who were at the World Trade Center site on September 11, 2001, and the days immediately following the 9/11 attacks.
Among NYC firefighters enrolled in the randomized FIREHOUSE (Food Intake Restriction for Health Outcome Support and Education) study who took part in a microbiome substudy, those who followed a low-calorie, Mediterranean-style diet had higher levels in stools samples at 6 months of Bacteroides ovatus, a bacterial species associated with protection against bowel inflammation.
In contrast, participants who followed a usual care diet had elevated 6-month levels of a species associated with high-fat diets and inflammation, reported Rachel Lam, a predoctoral fellow in the Nolan Lab at NYU Langone Medical Center in New York City, at the American College of Chest Physicians (CHEST) annual meeting here.
“Overall, we found that in our validation cohort, Bacteroides ovatus was increased in the LoCalMed arm after 6 months, and this bacterial species is associated with fewer negative health effects,” she said.
Lam noted that in a murine model of high-fat diets, mice gavaged with Bacteroides ovatus had reductions in body mass index and decreased serum LDL cholesterol and triglyceride levels.
FIREHOUSE Cohort
Senior author Anna Nolan, MD, whose lab members study predictors of lung function loss in a cohort of firefighters who were exposed to the particulate matter clouding the air of lower Manhattan on 9/11 and the ensuing days, told Medscape Medical News that the findings, while preliminary, support previous research findings on potential links between intestinal microbiota and lung function.
“It’s interesting that we saw this done in other models, like mouse models and such, where certain bacteria were viewed as healthy for the system, and if they were able to bring that bacteria out in larger amounts they saw anti-inflammatory effects, so we’re hoping to mirror that and also do a mouse model,” she said.
Nolan’s group has previously shown that markers for the metabolic syndrome, inflammation, and vascular injury detected in serum samples taken within 6 months of 9/11 were predictive for later abnormal lung function. In addition, their group has found that elevated serum levels of an LDL metabolite after intense World Trade Center dust exposure is a risk factor for future impaired lung function as measured by forced expiratory volume in 1 second (FEV1).
In the FIREHOUSE trial, 89 patients were randomly assigned either to a technology-supported educational and behavioral intervention targeting calorie restriction for weight loss while following a low calorie Mediterranean diet, or to usual care. The usual care arm included participants who were informed about their weight, BMI, and other standard measures at annual visits and were given general advice about healthy eating, but were not assigned to a specific diet.
Participants in the LoCalMed group had significant decreases in BMI and increases in FEV1 compared with those in the usual care group. In addition, the LoCalMed group had improved vascular health, better dietary habits, decreases in fats and calories from sweets, and decreases in inflammation as measured by a lower white blood cell count.
Microbiome Substudy
At CHEST 2023, Lam reported on microbiome pilot and validation substudies of FIREHOUSE.
The pilot study included five patients in each arm. The validation sample included 15 participants in the Mediterranean diet group and 16 in the usual care diet group.
Each participant’s microbiome was assessed with genomic sequencing with sequences aligned to a bacterial database. The number and diversity of bacterial species in each sample were determined with the Chao1 Index and Shannon Index, respectively.
There were no significant differences among the study groups in mean age, exposure at the World Trade Center site, or years of service.
Although bacterial diversity did not differ between the study arms either at baseline or at 6 months, in both groups it significantly decreased over time (P = .02 in the pilot, P < .0001 in the validation arm).
In the pilot study, there was an increase over 6 months in the usual care arm only of Bilophila wadsworthia, a species associated with high-fat diets and inflammation.
In the validation study, patients in the LoCalMed arm had significant reductions in Ruminococcaceae (P = .015) and increases in both Bacteroides ovatus (P = .03) and Alistipes shahii (P = .038), a recently identified species with uncertain protective or pathogenic potential.
In contrast, there were no significant increases in species in the usual care group, but there were significant declines in several other bacterial species; Lam, however, did not say whether these changes had clinical significance. “Future studies will assess microbial association with clinical outcomes,” Lam said.
Confounding Factors
Samuel Evans, MD, a pulmonologist at Straub Medical Center in Honolulu who
moderated the oral abstract session where the data were presented, commented that the data are interesting but added that associations are difficult to determine given the heterogeneity of exposures that firefighters encounter.
“I think it’s interesting that clearly diet is influencing the type of bacteria in the biome in the gut, and perhaps some are favorable, and some are not favorable,” he told Medscape Medical News. “We already know that the Mediterranean diet is associated with better health outcomes, so it makes sense, but can we tease out in the microbiome which bacteria are harmful and which are helpful.”
He noted that there a lot of confounding factors and that “it’s hard to find the right signal when you have so many variables.”
The FIREHOUSE study is supported by the CDC’s National Institute of Occupational Safety & Health and the National Heart, Lung, and Blood Institute. Lam, Nolan, and Evans report no relevant financial relationships.
American College of Chest Physicians (CHEST) 2023 Annual Meeting. Presented October 8, 2023.
CHEST. Published online October 8, 2023. Abstract
Neil Osterweil, an award-winning medical journalist, is a long-standing and frequent contributor to Medscape.
Source: Read Full Article