Researchers have uncovered the mechanism through which a single DNA base change dramatically raises the risk of a subform of type 2 diabetes (T2D) called metabolically obese normal weight (MONW). This genetic variant, which affects a gene called COBLL1, impinges a pathway that reduces the ability of subcutaneous adipocytes—fat cells under the skin—to accumulate and store lipids properly.
The findings are from scientists at the Broad Institute of MIT and Harvard, Massachusetts General Hospital (MGH), Technical University of Munich (TUM), Stanford University, and University of Chicago. They combined a series of computational and experimental strategies into a variant-to-function study tracing the variant’s effect to its target gene, relevant cell type, and cellular functions in individuals with MONW. The team describes their findings in a paper published in Nature Metabolism.
Many studies have linked obesity to T2D. However, while people classified as MONW (who may account for some 30 percent of normal-weight individuals in the general population) have the impaired insulin sensitivity of T2D (their cells struggle to properly respond to insulin), they also have normal body weight.
“MONW is an important example of how T2D actually represents a range of subforms with distinct biological and pathophysiological features,” said Melina Claussnitzer, an institute member at Broad, co-director of the institute’s Type 2 Diabetes Systems Genomics Initiative, and associate director of scientific strategy for the Novo Nordisk Foundation Center for Genomic Mechanisms of Disease at Broad; and co-senior author on the study with Marcelo Nobrega at the University of Chicago. “And despite how common it is, MONW and its underlying biology are just beginning to garner attention in the field.”
A prelude with a plot twist
Genome-wide association studies have identified more than 700 loci, or regions of the genome, associated with high blood-sugar traits and T2D, and more than 1,000 with obesity-related traits. A small number are associated with the MONW trait signature: reduced body fat, a decreased ratio of subcutaneous adipose tissue (fat tissue under the skin) to visceral adipose tissue (fat tissue deep inside organs and tissues), and an increased risk of insulin resistance and type 2 diabetes, reminiscent of lipodystrophy (a group of rare metabolic conditions marked by redistribution of body fat).
One such genomic region, the 2q24.3 locus, is located near a gene, GRB14, that encodes a docking protein that works with the insulin receptor.
“Everybody—including us!—first suspected that GRB14 would be the MONW target, because its protein sits close to the insulin receptor,” said Claussnitzer, who is also faculty in the Center for Genomic Medicine at MGH and a member of the Broad’s Metabolism Program and Diabetes Research Group. “But it turned out to be something completely different.”
To find genes driving the MONW phenotype, the team employed a variant-to-function framework Claussnitzer has been developing since she was a Ph.D. student for linking non-coding genetic variants to the genes they regulate, the cell types in which they are active, and the biological pathways they affect.
First, the team computationally homed in on a base change—from a cytosine to a thymine—at a single position within the 2q24.3 locus. Using CRISPR-based approaches, they then explored the change in several tissues and cell types, surprisingly finding that it had no effect on GRB14. It did, however, affect expression of COBLL1, a gene that “nobody in the field had heard of,” Claussnitzer noted.
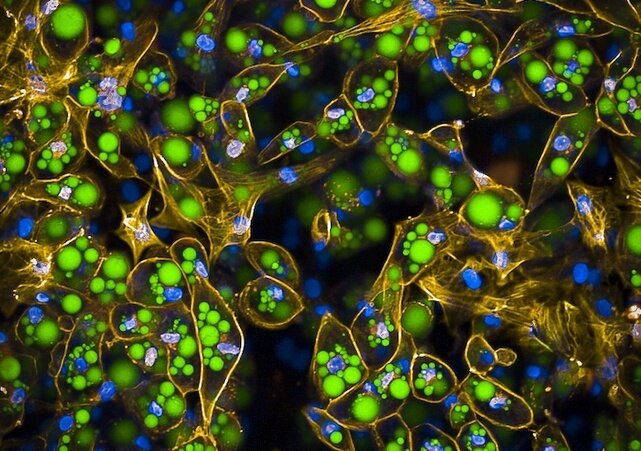
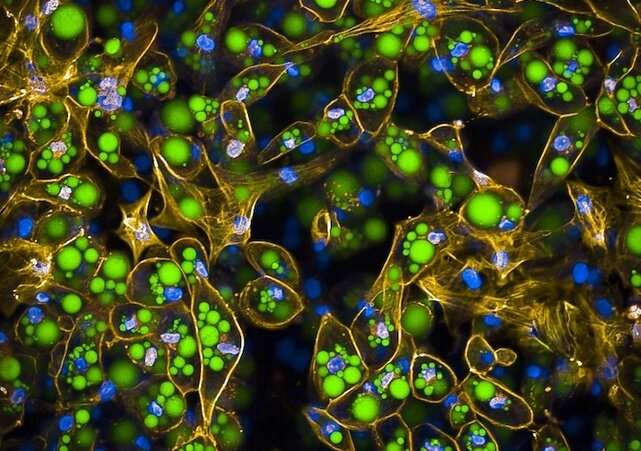
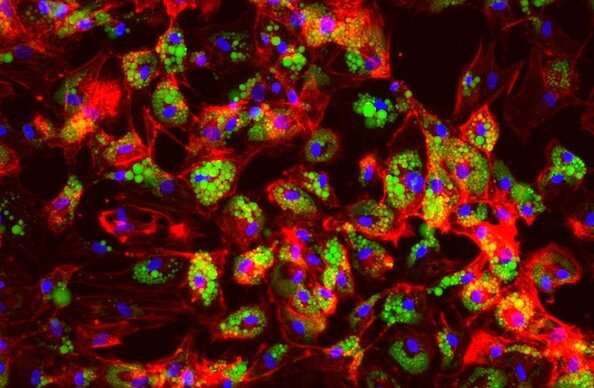
The team then altered COBLL1 expression in human adipocyte progenitor cells with gene knockdown experiments. By coupling the experiments with LipocyteProfiler, an imaging assay tailored for cardiometabolic disease research, they found that changes in COBLL1 expression alter how a developing fat cell’s cytoskeleton matures.
In normal adipocyte progenitor cells, actin cytoskeleton stress fibers congregate near the center of the cell. As the cell matures, it breaks those fibers down, allowing the cytoskeleton to migrate closer to the cell membrane. This makes room for fat-storing lipid droplets to form and grow, and supports metabolic processes such as insulin responsiveness and lipid metabolism.
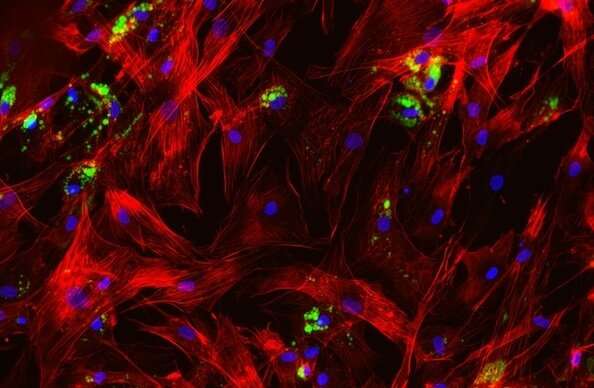
Following COBLL1 knockdown, however, the researchers saw that the stress fibers in subcutaneous adipocytes failed to degrade, preventing the cells from remodeling the cytoskeleton, which reduced their fat storage capacity. With the subcutaneous cells unable to store fat efficiently, it is redirected to visceral adipocytes or other tissues like the liver or the muscle, which can lead to severe insulin resistance.
“This COBLL1-downregulating variant renders subcutaneous fat cells insulin resistant and metabolically inactive,” Claussnitzer explained. “This strongly suggested to us that a lack of COBLL1 expression was responsible for MONW.”
Validation victories
To validate Claussnitzer and her colleagues’ findings, a team led by Nobrega’s University of Chicago lab generated a mouse model lacking COBLL1, isolated the adipocyte progenitor cells, and sent cell samples to the Broad. LipocyteProfiler analysis revealed the same defects in actin cytoskeleton remodeling and adipocyte metabolism that Claussnitzer’s team had seen in human cells.
“The mice showed what the humans showed: they’re lean and they’re insulin resistant,” said Claussnitzer. “It was a beautiful recapitulation of the predictions made by the genome-wide association study results we started with.”
Their findings have major therapeutic implications for people with the MONW phenotype, and Claussnitzer and her lab have been approached by pharmaceutical companies interested in developing drugs that modulate COBLL1 expression.
“I find it most exciting that a phenotype that is generally summarized as T2D can be partitioned into a subgroup where subcutaneous adipocyte depletion can be explained by a gene target and an intriguing mechanism of action,” said Claussnitzer. “It introduces a novel and clinically meaningful therapeutic hypothesis.”
More information:
Viktoria Glunk et al, A non-coding variant linked to metabolic obesity with normal weight affects actin remodelling in subcutaneous adipocytes, Nature Metabolism (2023). DOI: 10.1038/s42255-023-00807-w
Journal information:
Nature Metabolism
Source: Read Full Article