The American College of Gastroenterology issued updated guidelines for celiac disease diagnosis, management, and screening that incorporates research conducted since the last update in 2013.
The guidelines offer evidence-based recommendations for common clinical questions on topics that include nonbiopsy diagnosis, gluten-free oats, probiotic use, and gluten-detection devices. They also point to areas for ongoing research.
“The main message of the guideline is all about quality of care,” Alberto Rubio-Tapia, MD, a gastroenterologist at the Cleveland Clinic, in Ohio, told Medscape Medical News.
“A precise celiac disease diagnosis is just the beginning of the role of the gastroenterologist,” he said. “But most importantly, we need to take care of our patients’ needs with good goal-directed follow-up using a multidisciplinary approach, with experienced dieticians playing an important role.”
The update was published in the American Journal of Gastroenterology on January 1.
Diagnosis Recommendations
The American College of Gastroenterology assembled a team of celiac disease experts and expert guideline methodologists to develop an update with high-quality evidence, Rubio-Tapia said. The authors made recommendations and suggestions for future research regarding eight questions concerning diagnosis, disease management, and screening.
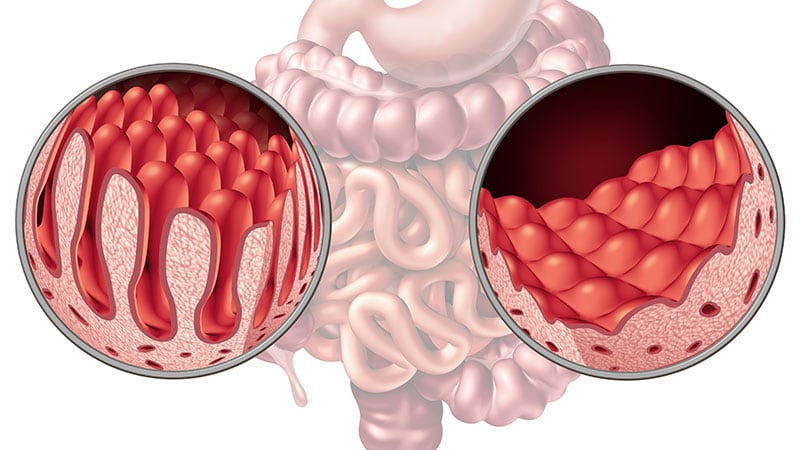
For diagnosis, the guidelines recommend esophagogastroduodenoscopy (EGD) with multiple duodenal biopsies — one or two from the bulb and four from the distal duodenum — for confirmation in children and adults with suspicion of celiac disease. EGD and duodenal biopsies can also be useful for the differential diagnosis of other malabsorptive disorders or enteropathies, the authors write.
For children, a nonbiopsy option may be considered to be reliable for diagnosis. This option includes a combination of high-level tissue transglutaminase (TTG) immunoglobulin A (IgA) — at greater than 10 times the upper limit of normal — and a positive endomysial antibody (EMA) finding in a second blood sample. The same criteria may be considered after the fact for symptomatic adults who are unwilling or unable to undergo upper GI endoscopy.
For children younger than 2 years, the TTG-IgA is the preferred test for those who are not IgA deficient. For children with IgA deficiency, testing should be performed using immunoglobulin G (IgG)–based antibodies.
Disease Management Guidance
After diagnosis, intestinal healing should be the endpoint for a gluten-free diet, the guidelines recommend. Clinicians and patients should discuss individualized goals of the gluten-free diet beyond clinical and serologic remission.
The standard of care for assessing patients’ diet adherence is an interview with a dietician who has expertise in gluten-free diets, the recommendations state. Subsequent visits should be encouraged as needed to reinforce adherence, the authors add.
During disease management, upper endoscopy with intestinal biopsies can be helpful for monitoring cases in which there is a lack of clinical response or in which symptoms relapse despite a gluten-free diet, the authors note.
In addition, after a shared decision-making conversation between the patient and provider, a follow-up biopsy could be considered for assessment of mucosal healing in adults who don’t have symptoms 2 years after starting a gluten-free diet, they add.
“Although most patients do well on a gluten-free diet, it’s a heavy burden of care and an important issue that impacts patients,” Joseph Murray, MD, a gastroenterologist at the Mayo Clinic in Rochester, Minnesota, told Medscape Medical News.
Murray, who wasn’t involved with this guideline update, contributed to the 2013 guidelines and the 2019 American Gastroenterological Association practice update on diagnosing and monitoring celiac disease. He agreed with many of the recommendations in this update.
“The goal of achieving healing is a good goal to reach. We do that routinely in my practice,” he said. “The older the patient, perhaps the more important it is to discuss, including the risk for complications. There’s a nuance involved with shared decision-making.”
Nutrition Advice
The guidelines recommend against routine use of gluten-detection devices for food or biospecimens for patients with celiac disease. Although multiple devices have become commercially available in recent years, they are not regulated by the US Food and Drug Administration and have sensitivity problems that can lead to false positive and false negative results, the authors note. There’s also a lack of evidence that the devices enhance diet adherence or quality of life.
The evidence is insufficient to recommend for or against the use of probiotics for the treatment of celiac disease, the recommendations state. Although dysbiosis is a feature of celiac disease, its role in disease pathogenesis and symptomatology is uncertain, the authors write.
Probiotics may help with functional disorders, such as irritable bowel syndrome, but because probiotics are marketed as supplements and regulations are lax, some products may contain detectable gluten despite being labeled gluten free, they add.
On the other hand, the authors recommend gluten-free oats as part of a gluten-free diet. Oat consumption appears to be safe for most patients with celiac disease, but it may be immunogenic in a subset of patients, depending on the products or quantity consumed. Given the small risk for an immune reaction to the oat protein avenin, monitoring for oat tolerance through symptoms and serology should be conducted, although the intervals for monitoring remain unknown.
Vaccination and Screening
The guidelines also support vaccination against pneumococcal disease, since adults with celiac disease are at significantly increased risk of infection and complications. Vaccination is widely recommended for people aged 65 and older, for smokers aged 19–64, and for adults with underlying conditions that place them at higher risk, the authors note.
Overall, the guidelines recommend case findings to increase detection of celiac disease in clinical practice but recommend against mass screening in the community. Patients with symptoms for whom there is lab evidence of malabsorption should be tested, as well as those for whom celiac disease could be a treatable cause of symptoms, the authors write. Those with a first-degree family member who has a confirmed diagnosis should also be tested if they have possible symptoms, and asymptomatic relatives should consider testing as well, they add.
The updated guidelines include changes that are important for patients and patient care, and they emphasize the need for continued research on key questions, Isabel Hujoel, MD, a gastroenterologist at the University of Washington Medical Center, told Medscape Medical News.
“In particular, the discussion on the lack of evidence behind gluten-detection devices and probiotic use in celiac disease addresses conversations that come up frequently in clinic,” said Hujoel, who wasn’t involved with the update. “The guidelines also include a new addition below each recommendation where future research questions are raised. Many of these questions address gaps in our understanding on celiac disease, such as the possibility of a nonbiopsy diagnosis in adults, which will potentially dramatically impact patient care if addressed.”
The update received no funding. The authors, Murray, and Hujoel have disclosed no relevant financial relationships.
Am J Gastroenterol. Published January 1, 2022. Full text
Carolyn Crist is a health and medical journalist who reports on the latest studies for Medscape, MDedge, and WebMD.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article