The innate immune system fights infectious agents, and the alarm messenger interferon plays a central role in this. However, if interferon is produced in the absence of an infection, it can lead to autoimmune diseases. Researchers at the University Hospital Bonn (UKB) and the Technical University (TU) Dresden have investigated an underlying mechanism and deciphered the driving force of uncontrolled interferon production through studying the rare autoimmune disease Aicardi-Goutières syndrome. Their study is published in the Journal of Experimental Medicine (JEM).
If our innate immune system recognizes viral genetic information by means of sensors, the alarm messenger type I interferon is produced. It is a very strong activator of immune cells and therefore essential in the defense against many pathogens, not only viruses. However, if too much interferon is produced, or if it is produced for too long, the overactivated immune system attacks healthy cells—collateral damage to what is actually a good immune response. In addition, the viral genetic information for the sensors looks for the most part like our own DNA and RNA.
In order to prevent such false recognition of our own genetic material, there are safety mechanisms in every cell. If these fail, interferon production occurs in the absence of viral infection leading to inflammation. This sterile inflammation, driven by uncontrolled innate immune activation, has been identified as one factor driving collagen diseases such as systemic lupus erythematosus (SLE).
“Diseases like lupus are difficult to study because many genes are involved. But the mechanism of interferon production as a result of the recognition of cell’s own nucleic acids also occurs in rare monogenetic autoimmune diseases and in which it can be precisely assigned to a gene defect,” says Prof. Dr. Rayk Behrendt, research group leader of the Institute of Clinical Chemistry and Clinical Pharmacology at UKB.
Recognition of DNA and RNA in cells is coupled
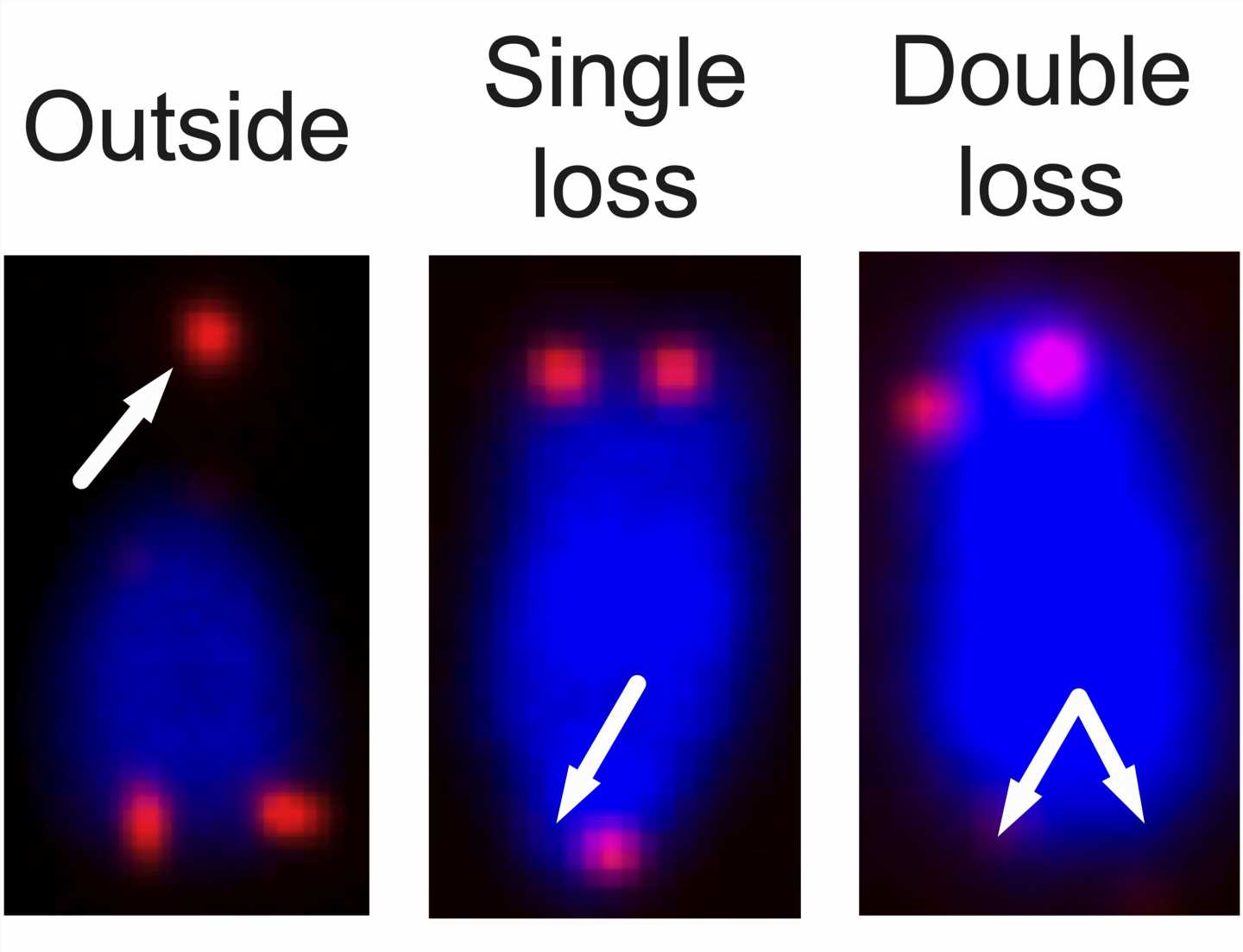
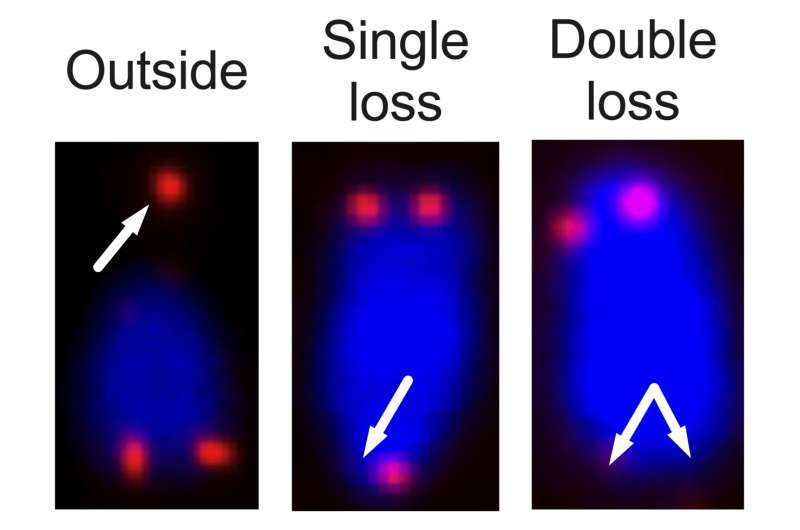
The research team from the medical faculties of the University of Bonn and the Technical University of Dresden took advantage of this and took a closer look at Aicardi-Goutières syndrome in a mouse model. This interferon-driven monogenetic autoimmune disease is triggered by inactivating mutations in genes that degrade cellular nucleic acids and thus prevent sensors of the innate immune system from being overactivated. One of these genes is called SAMHD1, and it regulates the replication and repair of DNA in the cell nucleus. Consequently, it was previously assumed that in affected individuals, DNA drives the disease.
“However, we now showed that contrary to previous expectations, recognition of cellular RNA is the driving force behind uncontrolled interferon production,” says Prof. Behrendt. “In this regard, it looks as if mainly RNAs from viruses encoded in our genome play a role. These sequences make up about 40 percent of our genetic material.”
Loss of DNA recognition suppresses the cellular immune system
But why was it thought for so long that DNA in SAMHD1-deficient cells activates the interferon system? It had been known for a long time that even healthy cells always produce a little interferon: so-called “tonic interferon signaling.” This leads to the fact that many gene products that act “antiviral” are always present in low concentrations and allow cells to quickly switch on an immune response. This includes many nucleic acid sensors, such as those that recognize RNA in the cytoplasm.
The research team observed that tonic interferon is activated via the DNA sensor cGAS, which recognizes cellular DNA, the carrier of our genetic information in the cell nucleus. If this DNA sensor is switched off, the cells become blind not only to DNA, but also to cellular or viral RNA. This is because the lack of tonic interferon reduces the amount of RNA sensors, which are part of the antiviral immune system.’
“So if you inactivate the DNA sensor cGAS in SAMHD1-deficient cells, it looks like DNA causes the disease because the interferon is gone. In reality, the cell simply can’t see the cell’s own unnatural RNA anymore,” says Tina Schumann, a post-doc at the Institute of Immunology at TU Dresden.
What are endogenous retroviruses doing in our cells?
Prof. Behrendt’s motivation to better understand the causes of this type of sterile inflammatory disease is to create novel approaches for therapies. For example, a deficiency in SAMHD1 appears to be a driver of cancer cell formation, among other things.
Therefore, the researcher from Bonn wants to clarify why the accumulation of RNA from endogenous retroviruses occurs in SAMHD1-deficient cells. In addition, he wants to clarify what activates cGAS in healthy cells and thus causes the basic alerting of the immune system, which is so vital for us.
More information:
Tina Schumann et al, Deficiency for SAMHD1 activates MDA5 in a cGAS/STING-dependent manner, Journal of Experimental Medicine (2022). DOI: 10.1084/jem.20220829
Journal information:
Journal of Experimental Medicine
Source: Read Full Article