Gut bacteria have a profound impact on health by aiding digestion, providing nutrients and metabolites, and working with the immune system to fend off pathogens. Some gut bacteria, however, have been implicated in progression of cancers of the gut and associated organs.
A new study by researchers from the University of Chicago shows that some commensal bacteria promote the development of leukemia caused by the murine leukemia virus (MuLV) by suppressing the animal’s adaptive anti-tumor immune response. When both the virus and commensal bacteria are present in mice, three genes known as negative immune regulators are expressed more, or upregulated, which in turn tamps down the immune response that would otherwise kill the tumor cells. Two of these three negative immune regulators are also known to be indicators of poor prognosis for humans with some forms of cancer.
“These two negative immune regulators have been really well documented to be poor prognostic factors in some human cancers, but nobody knew why,” said Tatyana Golovkina, Ph.D., Professor of Microbiology at UChicago and senior author of the study. “Using a mouse model of leukemia, we found that the bacteria contribute to upregulation of these negative immune regulators, allowing developing tumors to escape recognition by the immune system.”
Results of the research, “Gut commensal bacteria enhance pathogenesis of a tumorigenic murine retrovirus,” were published September 13 in Cell Reports.
Cancer is usually thought to be the result of spontaneous mutations that cause cells to grow and multiply out of control, forming tumors. In 1910, a pathologist named Peyton Rous took a sample from cancerous tumor in a chicken and injected it into a healthy bird, which developed cancer as well. His discovery was dismissed at the time, but researchers later discovered that the cancer was transmitted by a retrovirus. This discovery prompted more research and subsequent identification of numerous retroviruses causing various types of cancer.
Some cancer-causing retroviruses take advantage of gut microbes to spread and replicate. For example, in a 2011 study, Golovkina and her team found that a virus that causes mammary tumors in mice depends on gut bacteria, enabling the virus to block the immune responses from recognizing and eliminating infected cells. Thus, the microbes help the virus replicate and as a result, tumors develop.
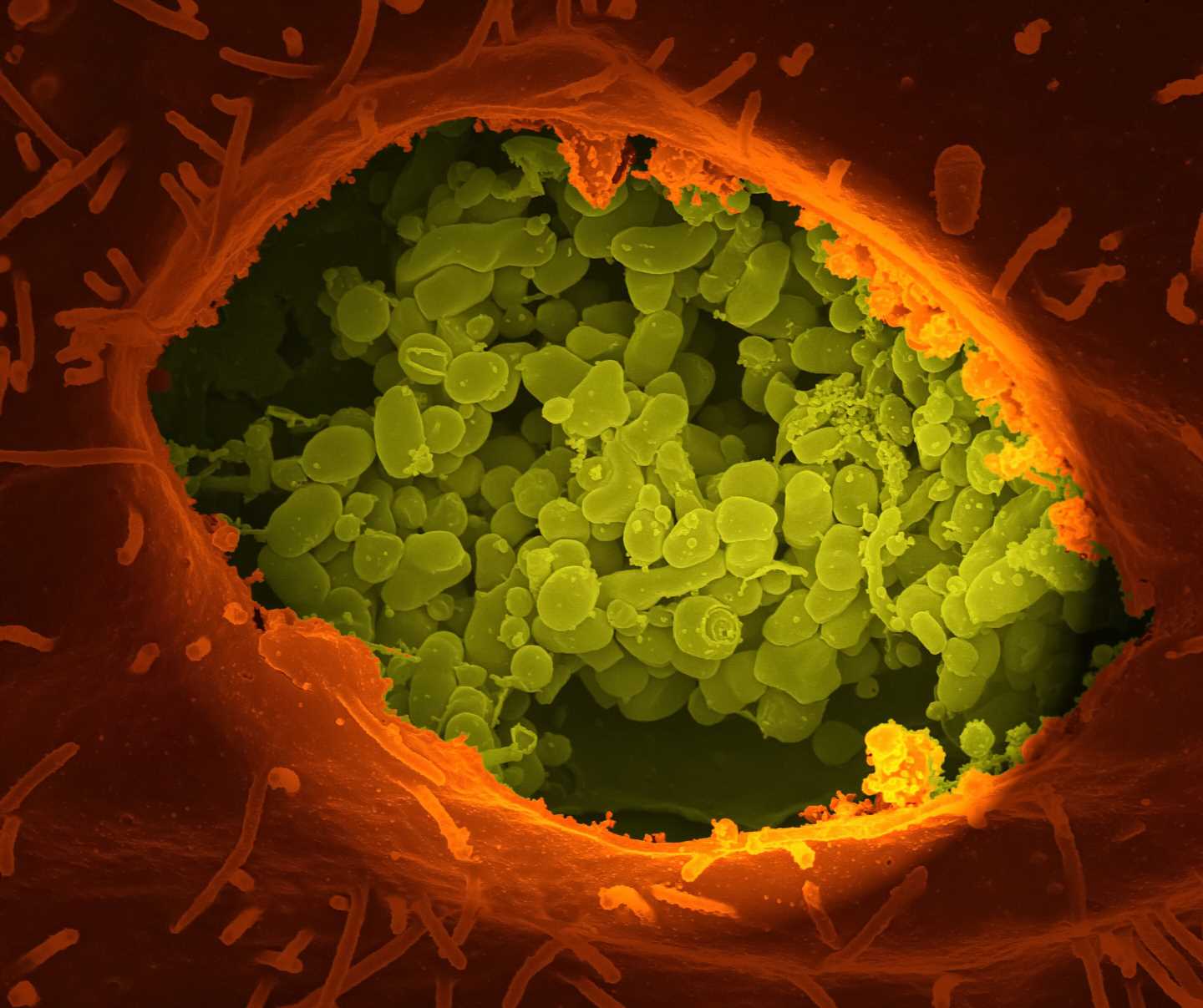
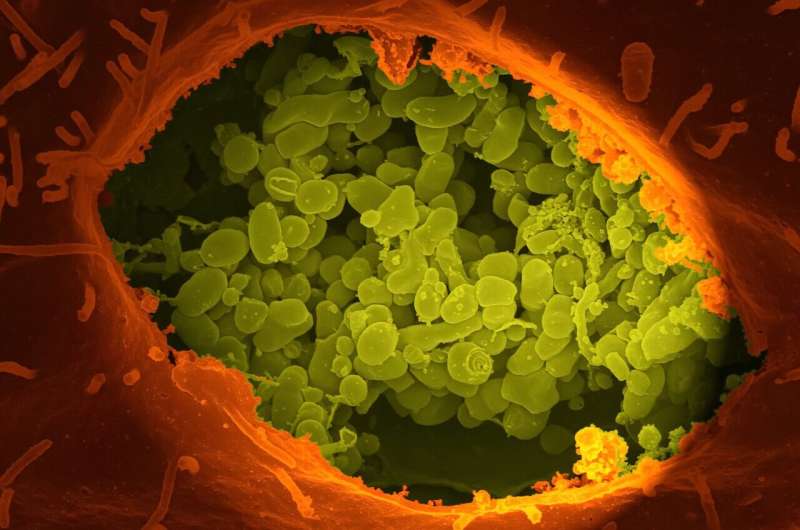
In the new study, the researchers wanted to see if commensal bacteria affected the development of a virus-induced cancer in another way besides assisting its replication. They used germ-free (GF) mice that had been raised in a special facility so they had no microbes, and specific pathogen free (SPF) mice that don’t have any pathogenic microbes that could causes disease but do have common commensal microbes, including bacteria that normally populate the gut. GF and SPF mice were both infected with the murine leukemia virus (MuLV). While the virus infected and replicated equally well in both types of mice, only SPF mice developed high-frequency tumors.
Virally induced cancer cells all express viral antigens, or molecules that mark them as foreign to the host and make them the targets for the immune attack. For the virally induced tumor cells to continue to replicate, they must be protected from the immune system’s attack, so, Golovkina’s team searched for a microbe-dependent immune evasion mechanism that enabled virally induced cancer cells to survive in the host.
The team performed a series of experiments with immunodeficient mice that were specially engineered, so they lacked the adaptive immune system. In the germ-free setting, these mice developed tumors when exposed to the virus with the same frequency as immunosufficient SPF mice with intact immune systems. So, the anti-tumor immune response was being counteracted by microorganisms, which were subsequently identified as commensal bacteria.
The researchers then found that commensal bacteria induced three genes known as negative immune regulators in infected mice. These genes normally act to shut down the immune system after it dealt with a pathogen, but in this case, they held back an immune response directed against cancer cells. Two of the three upregulated negative immune regulators—Serpinb9b and Rnf128—are also known to be indicators of poor prognosis for humans with some spontaneous cancers. Not all commensal bacteria had tumor promoting properties, so Golovkina and her team are continuing to research more on why this immune suppressing capability only comes into play when both virus and bacteria are present.
“Now we have to figure out what’s so special about bacteria which have these properties,” she said.
Source: Read Full Article