Researchers have created an inhalable COVID-19 vaccine that is shelf stable at room temperature for up to three months, targets the lungs specifically and effectively, and allows for self-administration via an inhaler. The researchers also found that the delivery mechanism for this vaccine—a lung-derived exosome called LSC-Exo—is more effective at evading the lung’s mucosal lining than the lipid-based nanoparticles currently in use, and can be used effectively with protein-based vaccines.
Ke Cheng, the Randall B. Terry Jr. Distinguished Professor in Regenerative Medicine at NC State and a professor in the NC State/UNC-Chapel Hill Joint Department of Biomedical Engineering, along with colleagues from UNC-Chapel Hill and Duke University, led the development of the vaccine prototype from proof-of-concept to animal studies.
“There are several challenges associated with vaccine delivery we wanted to address,” Cheng says. “First, taking the vaccine via intramuscular shot is less efficient at getting it into the pulmonary system, and so can limit its efficacy. Inhaled vaccines would increase their benefit against COVID-19.
“Second, mRNA vaccines in their current formulation require cold storage and trained medical personnel to deliver them. A vaccine that is stable at room temperature and that could be self-administered would greatly reduce wait times for patients as well as stress on the medical profession during a pandemic. However, reformulating the delivery mechanism is necessary for it to work through inhalation.”
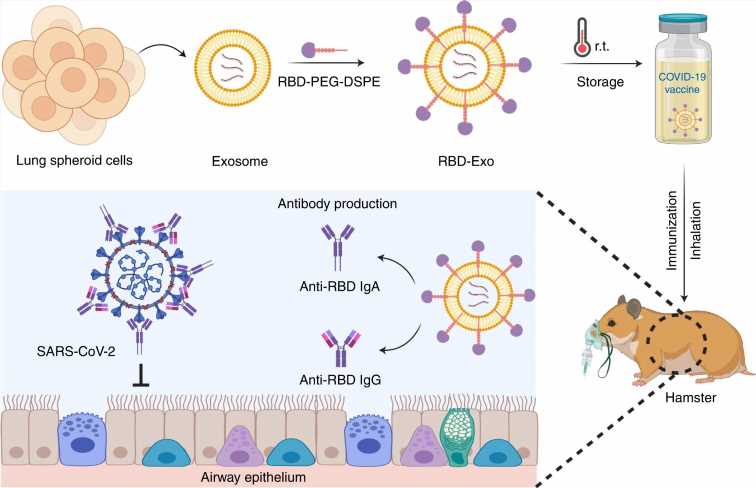
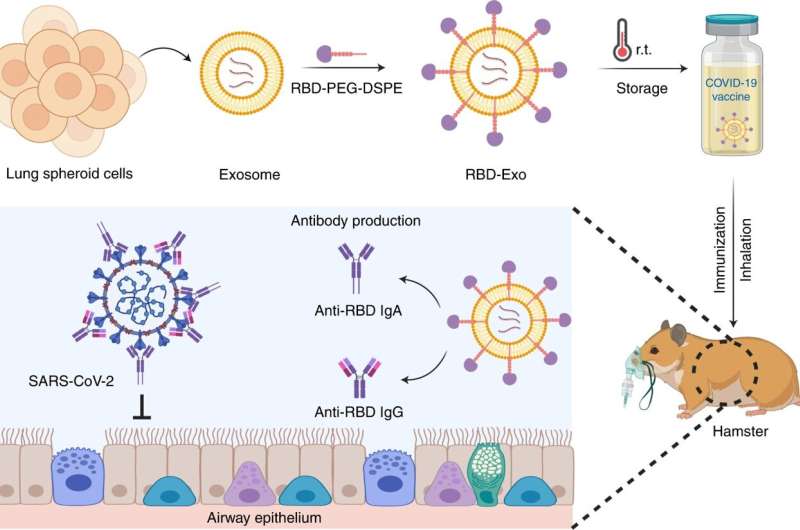
In order to deliver the vaccine directly to the lungs, the researchers used exosomes (Exo) secreted from lung spheroid cells (LSCs). Exosomes are nanosized vesicles that have recently been recognized as an excellent means of drug delivery.
First, the researchers looked at whether LSC-Exo was able to deliver protein or mRNA “cargos” throughout the lungs. The researchers compared the distribution and retention of LSC-Exo to nanoparticles similar to lipid nanoparticles currently used with mRNA vaccines. In a paper in Extracellular Vesicle, the researchers demonstrated that lung-derived nanoparticles were more effective at delivering mRNA and protein cargo to bronchioles and deep lung tissue than synthetic liposome particles.
Next, the researchers created and tested an inhalable, protein-based, virus-like particle (VLP) vaccine by decorating the exterior of LSC-Exo with a portion of the spike protein—known as the receptor binding domain, or RBD—from the SARS-CoV-2 virus. A paper describing the research is published in Nature Biomedical Engineering.
“Vaccines can work through various means,” Cheng says. “For example, mRNA vaccines deliver a script to your cell that instructs it to produce antibodies to the spike protein. This VLP vaccine, on the other hand, introduces a portion of the spike protein to the body, triggering the immune system to produce antibodies to the spike protein.”
In rodent models, the RBD-decorated LSC-Exo vaccine (RBD-Exo) elicited production of antibodies specific to the RBD, and protected the rodents, after two vaccine doses, from infection with live SARS-CoV-2. Additionally, the RBD-Exo vaccine remained stable at room temperature for three months.
The researchers note that while the work is promising, there are still challenges associated with large-scale production and purification of the exosomes. LSCs, the cell type used for generating RBD-Exo, are currently in a Phase I clinical trial by the same researchers for treating patients with degenerative lung diseases.
Source: Read Full Article