The study covered in this summary was published in medRxiv.org as a preprint and has not yet been peer reviewed.
Key Takeaways
-
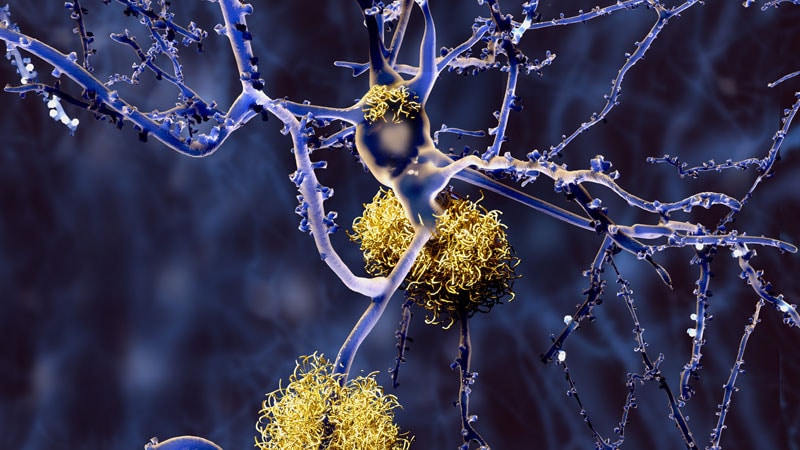
The clinical value of biologic criteria ― global amyloid burden (A), composite of temporal region of tau PET uptake (T), and presence of neurodegeneration (N) ― was confirmed to predict cognitive impairment in 580 cognitively unimpaired individuals across four cohorts.
-
The study demonstrated that Ab and tau PET positivity in cognitively unimpaired individuals is a substantial predictor of near-term progression to mild cognitive impairment (MCI) and longitudinal cognitive decline. The evidence of neurodegeneration implies substantial additional probability of clinical progression.
-
Abnormality in both Ab and tau PET was associated with a greater risk of near-term clinical progression than abnormality of Ab PET alone.
-
Clinical progression to MCI was observed in 32% to 83% of participants who had global amyloid burden (A+) and temporal region tau PET uptake (T+). In two cohorts, progression to MCI increased to 100% when neurodegeneration was present (N+). The data suggest that A+T+ individuals are on a pathway toward AD symptoms.
Why This Matters
-
The study assessed the clinical relevance of the National Institute on Aging–Alzheimer’s Association (NIA-AA) biological criteria for identifying individuals with preclinical Alzheimer’s disease (AD), given the lack of clarity on whether the AT(N) biological framework for AD can predict those at risk of developing AD-related cognitive impairment.
-
The study helped in determining a biological definition of preclinical AD. The biological definition of AD can help to identify individuals with preclinical AD who are candidates for disease-modifying therapies and help prevent AD progression. The study also helped define parameters for clinical trial recruitment and prognosis of patients with early clinical disease.
Study Design
-
The study assessed 580 individuals from four independent cohorts. These included the Pre-symptomatic Evaluation of Experimental or Novel Treatments for Alzheimer’s Disease (PREVENT-AD), the Harvard Aging Brain Study (HABS), the Australian Imaging, Biomarker, and Lifestyle (AIBL) study, and the Knight Alzheimer Disease Research Center (ADRC) dataset. All participants were cognitively unimpaired at the time of Ab and tau PET scan and were clinically observed for at least 1 year following scans.
-
Patients were stratified into four biomarker groups on the basis of binary assessment of global amyloid burden and composite of temporal region of tau PET uptake (A+T+, A+T-, A-T+, A-T-). The presence or absence of neurodegeneration (N+/N-) was assessed using temporal cortical thickness.
-
The primary outcome was clinical progression to MCI, identified by consensus committee review. A secondary outcome was cognitive decline, identified by slope >1 standard deviation below A-T- participants who did not experience disease progression.
Key Results
-
Across four cohorts, from 7.19% to 12.50% of participants were classified as A+T+. Of these individuals, 32% to 83% of A+T+ participants experienced progression to MCI. The mean progression time was 2.0 to 2.72 years. Of A+T+ individuals, in two cohorts, 100% of A+T+(N+) individuals experienced progression to AD symptoms. These results confirmed the clinical prognostic value of the NIA-AA research criteria.
-
In comparison with other PET biomarker groups, a greater proportion of A+T+ participants experienced progression to MCI (P < .001 across all groups). A hazard ratio of >5 was observed in the A+T+ group. In all other biomarker groups, fewer than 12% of participants experienced progression to MCI.
-
In all cohorts, A+T+ participants experienced greater longitudinal cognitive decline compared with other groups (P values < .03). A greater proportion of A+T+ participants who did not experience progression in PREVENT-AD and Knight ADRC showed cognitive decline (80% and 30.77%, respectively) compared with A+T- and A-T- groups. Many persons who were A+T+ and did not experience progression showed longitudinal cognitive decline, whereas in other groups, cognitive trajectories remained stable.
Limitations
-
The study was limited by the modest number of persons in the A+T+ group, although the sample size was similar to that of previous studies.
-
The maximum duration of clinical follow-up after PET varied among individuals and was short overall (median, 1.94 – 3.66 years).
-
The research framework for biological definition of AD uses dichotomous categories to define biomarker abnormality. In PET studies, the anatomic region used to define tau positivity is a matter of choice.
Disclosures
-
The study was supported by the Fonds de Recherche du Quebec Sante (FS), which is supported by the Canada First Research Excellence Fund.
-
The original article contains full disclosures of the authors’ relevant financial realtionships.
This is a summary of a preprint research study, “AT(N) Predicts Near-Term Development of Alzheimer’s Disease Symptoms in Unimpaired Older Adults,” written by researchers at McGill University, Department of Psychiatry, Montreal, Canada, the Douglas Mental Health University Institute, Montreal, Canada, and the AIBL, Knight ADRC, HABS, and PREVENT-AD research groups, published on medRxiv and provided to you by Medscape. This study has not yet been peer reviewed. The full text of the study can be found on medRxiv.org.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article