In a recent study published on the medRxiv* preprint server, researchers estimate the impact of the coronavirus disease 2019 (COVID-19) pandemic on cardiovascular disease (CVD) and its management in England, Scotland, and Wales using dispensed CVD medication data.
As CVD continues to be the most common cause of mortality and morbidity worldwide, it is vital to understand the impact of the ongoing COVID-19 pandemic on CVD and its risk factors. The need for this information is also due to the lack of understanding of the downstream impact of missed detection of the incident CVD cases.
Study: The adverse impact of COVID-19 pandemic on cardiovascular disease prevention and management in England, Scotland and Wales: A population-scale descriptive analysis of trends in medication data. Image Credit: Lisa-S / Shutterstock.com
About the study
The current study was the first to report the impact of the COVID-19 pandemic on the management of CVD using anonymized individual-level population-scale data for 1.32 billion records of dispensed CVD medications across 15.8 million people in England, Scotland, and Wales. The study examines data of medications dispensed from April 1, 2018, to July 31, 2021, to both male and female patients between the ages of 18 to 112 years at pharmacies in all the nations.
The study provides a comprehensive quantification of the reduction in the control of CVD risk factors. Furthermore, the authors investigate the impact of not treating CVD and its risk factors on future CVD events by examining changes in the dispensed medicines used to treat CVD and CVD risk factors throughout the COVID-19 pandemic. The researchers investigated the trends in dispensed CVD medications stratified by individual demographic characteristics such as age, sex, region, or ethnicity.
For the study period of March 2019 to May 2021, dispensed medications for CVD conditions that could be modified by antihypertensives, lipid-lowering, type-2 diabetes (T2DM), and insulin medications were included.
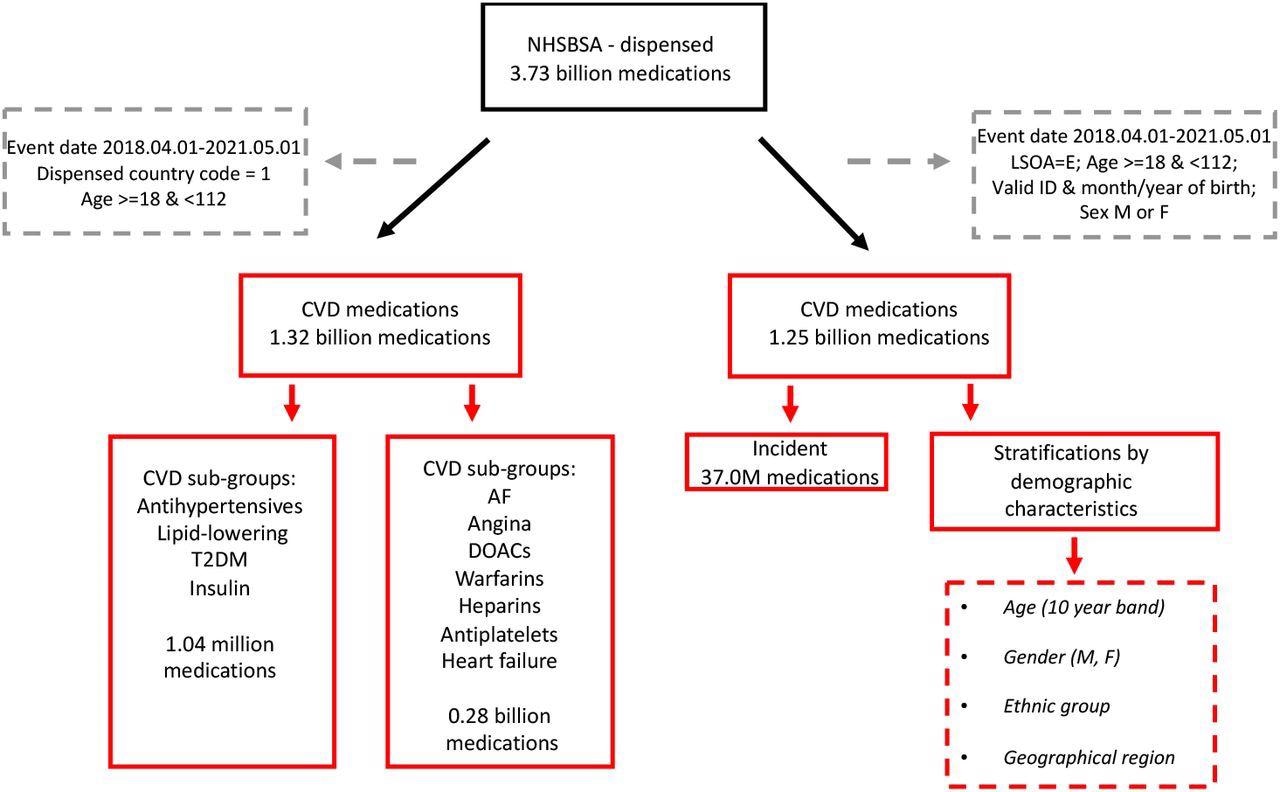
Flowchart showing selection of analytical datasets from NHSBSA (England)
Study findings
In England, year-on-year CVD medicine dispense rates per person increased from 26.0 to 27.0. Contrastingly, in Wales, these rates fell from 32.8 to 32.0, while in Scotland, these rates increased stably from 0.4 to 18.9 medicines per person per year.
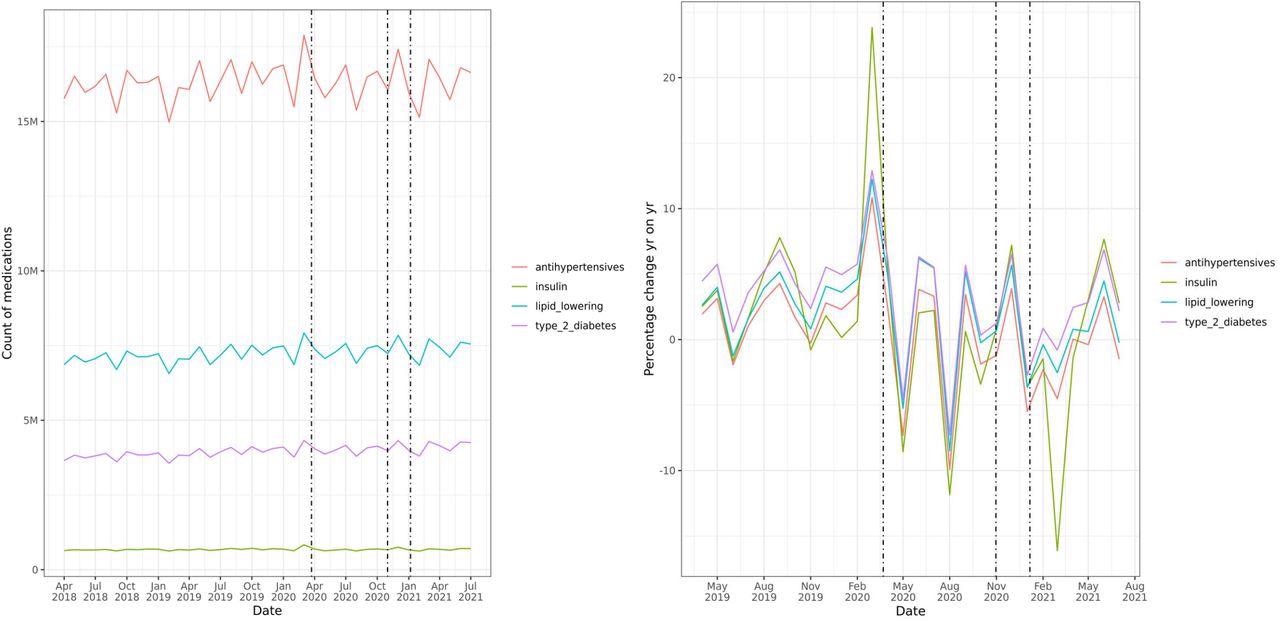
Trends in dispensed CVD medicines over course of pandemic by CVD/ CVD risk factor sub-groups; i) counts by month, and ii) percentage change year-on-year by month; including England, Scotland and Wales. Footnotes: Dotted lines indicate timing of first, second and third national lockdowns: 26th March 2020, 5th November 2020 and 6th January 2021 respectively
A downward trend in the annual percent change in CVD medicines dispensed throughout 2020 and 2021 indicated a decline in the active management of CVD in the population. Across all the CVD sub-groups, a sharp growth in year-on-year medicines dispensed in the pre-pandemic period was followed by a decline below the 2019 levels in May 2020.
Interrupted Time Series (ITS) analysis evaluated prescription trends from April 2018 to May 2021 by individual CVD sub-groups at weekly timepoints during the COVID-19 pandemic in England. The results showed a sharp increase in the prescription of CVD medicines before the first national lockdown.
In contrast, the period between the first (January 5, 2020) and second national lockdowns (January 6, 2021) witnessed declining CVD prescriptions, which did not increase in the four weeks preceding the second lockdown.
During the times preceding the first national lockdown, the highest year-on-year rise in dispensed medicines was observed in the age group of 18-29 and 30-39 years, and the pattern did not change for both males and females. During the same time period, England, Yorkshire, and the Humber saw the highest year-on-year increase in dispensed medicines with peaks in June-September reflecting additional local restrictions at those times. Similar trends were observed in Scotland and Wales, with a marked change in year-on-year dispensing associated with the first COVID-19 lockdown.
As compared to pre-pandemic times, the incident medicine dispensing for antihypertensives, lipid-lowering, and T2DM medications decreased in the immediate post-pandemic period. In May 2020, there was a slow recovery in incident prescriptions; however, this recovery plateaued during the second and third national lockdowns.
Subsequently, there were on average 23,909 and 14,792 fewer patients on antihypertensives and lipid-lowering medications respectively. Comparatively, 1,642 more patients were reported to be prescribed T2DM medications per month during the first half of 2021 as compared with the same months in 2019.
Hypertension is the most common CVD risk factor for which medicines are prescribed. Using a cost-effective National Institute of Health and Care Excellence (NICE) analysis model, the researchers estimated that the missed antihypertension treatment could have resulted in 13,659 additional CVD events if people were left untreated, including 2,281 and 3,474 more myocardial infarctions (MIs) and strokes, respectively.
Conclusions
Overall, the study results indicate that year-on-year changes in dispensed CVD medicines by month substantially increased to 11.8% in March 2020 before the first, but not during subsequent, COVID-19-induced lockdowns in the U.K. Therefore, 491,203 fewer individuals initiated antihypertensive treatment across England, Scotland, and Wales from March 2020 to the end of May 2021, as compared to 2019.
The study also highlighted the indirect socio-economic impact of the COVID-19 pandemic in the U.K. by demonstrating that the management of CVD risk factors as proxied by incident use of CVD medicines has not returned to pre-pandemic levels. Therefore, novel methods to identify and treat individuals who have missed CVD treatment are urgently required to avoid large numbers of future CVD cases.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Dale, C. E., Takhar, R., Carragher, R., et al. (2021). The adverse impact of COVID-19 pandemic on cardiovascular disease prevention and management in England, Scotland and Wales: A population-scale descriptive analysis of trends in medication data. medRxiv. doi:10.1101/2021.12.31.21268587. https://www.medrxiv.org/content/10.1101/2021.12.31.21268587v1
Posted in: Medical Research News | Medical Condition News | Disease/Infection News | Healthcare News
Tags: Cardiology, Cardiovascular Disease, Coronavirus, Coronavirus Disease COVID-19, Diabetes, Insulin, Medicine, Mortality, Pandemic

Written by
Neha Mathur
Neha Mathur has a Master’s degree in Biotechnology and extensive experience in digital marketing. She is passionate about reading and music. When she is not working, Neha likes to cook and travel.
Source: Read Full Article