On a Friday afternoon this past December, more than 130 scientists gathered on a Zoom meeting to talk about Omicron, the latest SARS-CoV-2 variant of concern, which has ripped across the globe with ferocious infectivity.
The collection of names and faces on the call spanned disciplines—virology, epidemiology, infectious diseases, immunology, computational biology, critical care medicine; it spanned institutions—Harvard Medical School, Massachusetts General Hospital, Brigham and Women’s Hospital, the Broad Institute, Boston University, the University of Massachusetts; it spanned countries—the United States, South Africa, Botswana, England, and India.
Questions that sparked rounds of discussion that day included: Where did Omicron come from? Is it more capable of dodging immune defenses? Is it more virulent than prior variants? How will vaccines and treatments hold up against it?
At the writing of this story, Omicron has peaked in many places, a sister subvariant (BA.2) has started gaining foothold, and some of these questions have been answered.
Yet, the questions raised on that call matter beyond Omicron. They will be the same unknowns that scientists may face with any variants should they arise. In that sense, Omicron may not be the end of the virus’s evolutionary story, but merely a twist in the plot.
Untangling the evolutionary maneuvers of the shapeshifting virus is the mission of the viral variants research group of the Massachusetts Consortium on Pathogen Readiness, an international scientific effort led by Harvard Medical School that was established in March 2020 to address both the immediate and long-term challenges of the COVID-19 pandemic and to enhance preparedness for future ones.
MassCPR researchers Jake Lemieux and Jeremy Luban, who co-lead the viral variants group, and their colleagues have hosted these international, multi-institutional, multidisciplinary Zoom calls every week in an effort to map the virus’s changing biology and behavior, to unravel how its newly acquired features may alter the way the virus interacts with its human host, and to glean clues about the virus’s evolutionary future.
“The complex questions we deal with involve the whole range of expertise from patient care to atomic structure,” said Luban, who is professor of molecular medicine, biochemistry & molecular pharmacology at UMass Medical School. “These calls have all of these experts working together, educating each other about their respective fields.”
“The pandemic has brought the community together in very concrete ways, and some of that will probably remain long after,” said Lemieux, who HMS instructor in medicine and an infectious disease specialist at Mass General. “The barriers to working together across labs, across institutions, across geographic regions are much lower than they ever have been.”
Broadly speaking, the overarching questions for the group are: How will the virus evolve? What will the consequences be? What can we do about it?
How will the virus evolve: The past as prolog?
There is an adage in human psychology that the best predictor of future behavior is past behavior. This may also be true in the case of viruses—up to a point. Knowing a pathogen’s evolutionary history is important, but not sufficient, to predict where it may be headed. SARS-CoV-2’s evolutionary track record is too short to provide meaningful insight about its future. And the virus’s record thus far has underscored its unpredictable nature.
Could clues come from other coronaviruses? Perhaps, but not very reliable ones, Luban and Lemieux warn, since each coronavirus is its own entity, making it challenging to draw broader comparisons.
“Some of the comparators for SARS-CoV-2 would be SARS-CoV-1 and MERS-CoV, which are related viruses that have infected people,” Luban said. “They are good examples of how impossible it is to predict where we’re headed because SARS-CoV-1 became extinct, and MERS-CoV has a totally different mode of infection and persists in an animal reservoir.”
Another factor that makes forecasting difficult is the relative scarcity of preexisting knowledge on coronaviruses. The world entered the COVID-19 pandemic with only a handful of coronavirus experts, Luban said. Interest in this field, as well as research funding for it, peaked in the mid-2000s after the first SARS outbreak, but quickly waned thereafter, leaving the scientific community with some serious blind spots. One of them turned out to be SARS-CoV-2’s propensity for mutation.
Mutations are a normal part of a virus’s life cycle. They occur when a virus makes copies of itself. Many of these mutations are inconsequential, others are harmful to the virus itself and yet others may provide it with a competitive advantage.
In early 2020, the assumption—and hope—was that SARS-CoV-2 would not change too fast. Like other coronaviruses, it has a mechanism that prevents too many changes, or errors, on the viral genome during replication.
“The virus has proofreading machinery unique to coronaviruses, and so the word on the street was these viruses were not as error-prone as other RNA viruses like poliovirus, influenza virus or HIV-1,” Luban said.
Indeed, early in the pandemic, SARS-CoV-2 accumulated about two mutations per month—a slow rate of change, which supported the initial forecast that SARS-CoV-2 would be a sluggish mutator.
Yet, a small minority of scientists, Luban included, were not as sanguine. In March of 2020, Luban began to pore over data from the 1918 influenza pandemic. He came across a striking chart showing three major spikes in deaths in the UK over the course of 1918 and 1919, a possible indicator of repeated cycles of infection caused by new viral variants.
“Could this be where we are headed with SARS-CoV-2?” Luban wondered.
He posed the question to influenza experts and epidemiologists around the world. Many got downright angry for even suggesting that possibility, a response Luban and Lemieux say may have been driven by a well-intentioned, if misplaced, impulse to reassure people and avoid being alarmist.
“The thing is if you are saying the house is not on fire, most of the time you’re right—the house isn’t on fire,” Lemieux said. “But sometimes when the fire alarm goes off, the thing to do is evacuate the house.”
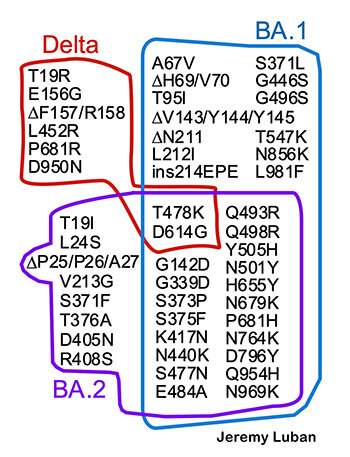
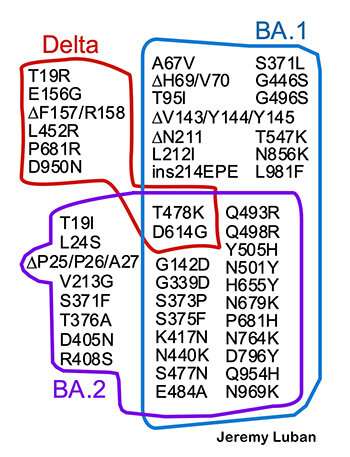
Luban’s suspicions were amplified by the appearance of some ominous changes in SARS-CoV-2’s genome. One of these changes was a mutation that changes the spike protein called D614G. Luban had noticed it because it reminded him of mutations he had studied in Ebola virus in two previous outbreaks—single amino acid swaps in the protein machinery that the virus uses to invade human cells. This suggested to Luban and a handful of like-minded colleagues that this mutation might be an adaptation that could increase SARS-CoV-2’s infectivity—just like the analogous change had done for Ebola virus.
In autumn of 2020, alpha—the first variant of concern—entered the scene, setting off waves of disease and death across the globe.
“There appeared a creature with maybe 10 times more mutations than had been seen in any previous strains from the pandemic up to that point,” Luban said. “It swept through the planet and took over, and all of a sudden the conversation changed.”
Since then, new variants have emerged: beta, gamma, delta, Omicron. And the cycles of infections, hospitalizations, and deaths have continued, not unlike the waves of death during the 1918-1919 influenza outbreak that captured Luban’s attention.
This has become a pandemic of variants, Lemieux said. They emerge, they are identified, and they are characterized in humans and in animal models. Monoclonal antibody therapies are now customizable to variants, and eventually vaccines might be calibrated to variants.
“It’s crazy to think how far we’ve come and how much the pandemic is the variants,” Lemieux said.
Some clues about the virus’s evolutionary future may come from Omicron’s past. While the provenance of Omicron remains a matter of scientific speculation that will likely never be resolved, researchers have four origin theories that apply as much to Omicron as to the previous variants of concern.
What this means is that any one of these origin mechanisms could also give rise to the next variant.
The first theory revolves around keystone mutations that may have enabled other mutations to accumulate. Luban describes these as mutations that by themselves may not be all that significant for a variant’s transmissibility but may be critical enablers of other important mutations. Case in point: D614G is a keystone mutation. Without it, alpha, beta, and gamma variants would have not occurred.
Such keystone mutations have and will likely become a permanent feature of the viral evolution, Luban said, and could lead to the emergence of new variants.
A second hypothesis posits that for the past two years, Omicron may have flown under the radar, with mutations accumulating undetected in parts of the world where diagnostic tests, genomic sequencing and vaccines are not widely available. That possibility exists for any future variants.
A third possibility is a spillover event from a human into another animal host, where SARS-CoV-2 replicated and acquired a constellation of genomic changes before it leapt back into a human host.
Yet another scenario emanates from the work of HMS’ Jonathan Li. Last year, Li described the case of an immunocompromised patient who was continuously infected with SARS-CoV-2 for five months. Throughout the infection viral evolution and major mutations were ongoing in the patient. Since this milestone report, other researchers have reported similar cases of viral evolution and mutation in patients with chronic SARS-CoV-2.
Lemieux and Luban note that many of the mutations that emerged in alpha, beta, gamma, delta, and Omicron had been previously noted in individuals with chronic SARS-CoV-2 infections and thus unable to clear the virus. In a newly published commentary, they say these chronic infections could offer a preview into future variants and should be regularly mined for emerging mutations.
What will the consequences be?
Middle-school biology lessons may have left many of us with a somewhat simplistic impression of evolution as a strategically selective process. But, in truth, evolution is often chaotic. This feature makes it challenging to predict the evolutionary trajectory of a pathogen.
“I think anybody who has an overarching theory that applies in all cases is likely to be wrong. Nature is not simple. There are many different types of hosts, many types of reservoirs, and many events that are not easily predicted by models,” says Jake Lemieux.
The two major forces of evolution are selection and drift, Lemieux says, and both of them are subject to randomness and chance.
“Selection is a deterministic force, but one played out in a probabilistic context, where you have something that tends to increase or decrease fitness, but that’s not the only thing that determines whether it’s passed on—there are lot of chance forces,” Lemieux said.
Genetic drift, on the other hand, is representative of random forces in evolution akin to the luck of the draw.
“If a mutation gets lucky and it just so happens that it occurs in an individual involved in a superspreading event, that mutation, in a sense, was lucky because due to chance alone it got passed into a large number of people,” Lemieux said.
This is why researchers cannot say that the pandemic is going to play out one way or another.
“We don’t know and probably we’ll never know what’s going to happen, it’s not like we have a source of viral variants that we can just monitor and see what’s coming,” Lemieux said. “We live next to this volcano that we can’t see, and we don’t know when it’s going to erupt.”
Yet, even within the context of uncertainty, there are some scenarios that are more likely than others.
One, and a highly unlikely one, is that the virus could just peter out into extinction.
“It’s extremely unlikely at this point that SAR-CoV-2 is going to disappear in a meaningful way. That ship has sailed,” Lemieux said.
For the virus to disappear now, it would have to vanish independently from every place around the globe, in every reservoir, Lemieux said, adding that this is “not likely to happen unless there’s some new vaccine technology that all of a sudden induces sterilizing immunity, which is possible. But I don’t think it’s on the horizon in the next couple of years.”
Another scenario involved a state of immunological equilibrium between virus and host. Support for this notion comes from the history of SARS-CoV-2’s more distant evolutionary cousins—four common human coronaviruses that have circulated for centuries, are endemic, and infect most people by the time they reach 18, causing mostly mild infections. These human coronaviruses are far older than SARS-CoV-2’s youngest and most closely related relatives, SARS-1 and MERS.
“We don’t know where these coronaviruses came from,” Luban said. “Were they always there or did they appear and wreak havoc initially like SARS-CoV-2 has?”
This is pure speculation, Luban added, but it is plausible that these four viruses at some point in history jumped into people and caused a lot of damage initially before reaching a state of equilibrium.
“Could SARS-CoV-2 be headed in that direction?” Luban says. “There is a historical precedent in virology for this scenario.”
Long-term attenuation could also be a factor of time. As each new generation gets vaccinated or encounters the virus early in life, humans may build longer-lasting protection than those who first encounter the virus as adults. It is unclear how long immunity to SARS-CoV-2 lasts, but history offers some examples that age at initial encounter could be a decisive factor in the longevity of immune memory.
“There are a lot of viruses that you get as a kid, which are annoying, maybe severely unpleasant, like chicken pox, that you really don’t want to get as an adult because the consequences are very different,” Luban said. “The age when you encounter a virus first really changes the outcome.”
Yet another possibility might be a gradual loss of virulence. Indeed, one of the most frequently asked questions is whether pathogens tend to lose their virulence over time independent of the host’s immune defenses.
“There are people who like that idea, who could find an example or two in history,” Luban said. “But I think if you poll the people who study it most deeply, they are not so sanguine about it. There’s no a priori reason why a virus should become less pathogenic so long as there are susceptible people for it to infect. If it kills off a billion people, there are still 6 billion hosts left. It doesn’t really matter to the virus.”
“I think anybody who has an overarching theory that applies in all cases is likely to be wrong,” Lemieux said. “Nature is not simple. There are many different types of hosts, many types of reservoirs, and many events that are not easily predicted by models.”
One such hard-to-predict event would be genetic recombination, which represents yet another possible evolutionary development, one that could take a benign or ominous turn, depending on what new features the virus acquires when combining with another one.
Recombination could come in two forms—a melding of two SARS-CoV-2 variants (delta marries Omicron) or a mash-up of two separate viruses. In the latter, SARS-CoV-2 and another respiratory virus could exchange genetic material during replication inside a host cell and spawn an entirely new virus. But because viral recombination between two viruses can occur only during replication inside a host cell, SARS-CoV-2 would have to encounter another virus replicating in the exact same cell at the exact same time.
Under another scenario, virus and host would reach a truce with periodic waves of widespread infection and spikes in disease severity. Given that SARS-CoV-2 has an endless reservoir of possible mutations and therefore new variants, there may be periodic eruptions in infections, but the degree of preexisting immunity would keep most people mildly infected and out of the hospital.
“The impression we are starting to get is that the immunity to stay out of the hospital and to stay alive may cross over many of the variants,” Luban said. “Much of the data we have suggest that is going to be the case. What preexisting immunity does not appear to do is completely prevent any symptomatic infection.”
“I think we’re going to see a trend toward more of a seasonality, a virus that has a lower impact on humans when it does flare up, but I think it’s also likely there will be flare-ups because of changes in transmissibility or immune escape or other things,” Lemieux said.
Regardless of which scenarios end up occurring, experts say, there is a 100 percent certainty that at least two things must occur to prepare humanity better for the next variant and, indeed, the next pathogen: proactive surveillance and global immunization.
What can we do, moving forward?
Even in the context of such great uncertainty, there are “known knowns,” meaning there are steps that scientists and policymakers can take to minimize damage from even the least favorable scenarios.
“Nobody knows where SARS-CoV-2 is headed, but the one thing that we do know for sure is that as long as there are unvaccinated people, variants with new clinical properties are possible and may plague us for years to come,” says Jeremy Luban.
The first thing, Lemieux said, is to do more sequencing of viral samples to monitor the genetic diversity of SARS-CoV-2 and detect emerging mutations—something the world has gotten better at with many countries now sequencing large proportions of samples in real or near-real time.
Second, look at the data. This is something the viral variants group is doing every Friday—looking at the data and asking what’s on the horizon and what should we be worried about.
But efforts must go beyond sequencing and trend analysis, Lemieux said.
There is an urgent need to develop a systematic early-warning system that would analyze surveillance data and identify genetic lineages that are more transmissible. More importantly, such a system would serve to predict transmissibility of new lineages as or before they emerge.
One such example is a model based on work co-led by Lemieux, Fritz Obermeyer, and Pardis Sabeti at the Broad Institute. The model, called PyR0 (“py-R-nought”), built using the probabilistic programming language Pyro, uses machine learning to analyze all of the sequencing data gathered worldwide to gage the relative transmissibility of variants across regions and across space and time.
This can help explain how the virus is becoming systematically more transmissible over time. The model can predict how fast a new lineage might spread based on its mutational profile and identifies viral lineages of concern as they emerge, which in turn can help determine which mutations look suspicious enough to test in the lab and be checked for increased infectivity or pathogenicity.
Such an approach can yield relative ranking of variants of concern so that scientists can identify emerging ones that seem to spread faster than others and certain ones that are likely to die out.
Eventually, however, scientists would need to develop a priority system that could help them distinguish between dangerous variants and those that just need watchful observation.
“At some point, we’re going to have to back off,” Lemieux said. “It is going to have to be a transition where sequencing becomes a part of the toolkit, but we also don’t overreact to everything we find when sequencing.”
Even the most sophisticated epidemiological tracking approaches will not be sufficient to get a handle on the contagion if they are not complemented by widespread vaccination.
To achieve that, it is critical to ensure equitable global access to vaccines in a way that allows for the synchronous immunization of large swaths of the human population over a short period of time, Luban and Lemieux say.
Viral variants arise from mutations that can occur under a variety of scenarios, but large numbers of immunologically naive hosts are the virus’s ultimate playground and a fountain of new mutations.
Vaccines, which boost host immune defenses and prevent or minimize viral replication, offer a critical tool to deprive the virus of opportunities for mutation. The more people are vaccinated, the less chance for the virus to find and exploit nonimmune hosts for its own advantage.
“Nobody knows where SARS-CoV-2 is headed,” Luban said. “But the one thing that we do know for sure is that as long as there are unvaccinated people, variants with new clinical properties are possible and may plague us for years to come.”
As the public health maxim goes, no one is safe until we are all safe.
Source: Read Full Article