Knees and hips wear out. Backs and necks become unstable. Fortunately, orthopedic surgeons specialize in musculoskeletal repair. And surgeries that formerly required open exposure are now accomplished with minimally invasive techniques. Surgical risks are reduced, as are postoperative pain and recovery time.
Orthopedic surgery is among the most common types of surgery, especially in developed countries with aging populations. In the US alone, surgeries for spinal fusion and knee or hip replacement amount to more than a million cases each year.
Imaging methods such as endoscopy, CT scanning, and infrared navigation assist surgical planning and provide visual or spatial guidance, yet the full potential of optical sensing in orthopedic surgery remains to be explored. Researchers from the Biophotonics@Tyndall group at Ireland’s Tyndall National Institute (TNI) teamed up with coauthors from Sunnybrook Health Sciences, University of Toronto, South Infirmary Victoria University Hospital, and University College Cork, to offer a perspective on the integration of optical sensing into orthopedic surgical devices, published in the Journal of Biomedical Optics. They describe how optical sensing, via spectroscopy or imaging, might address unmet clinical needs in orthopedic surgery.
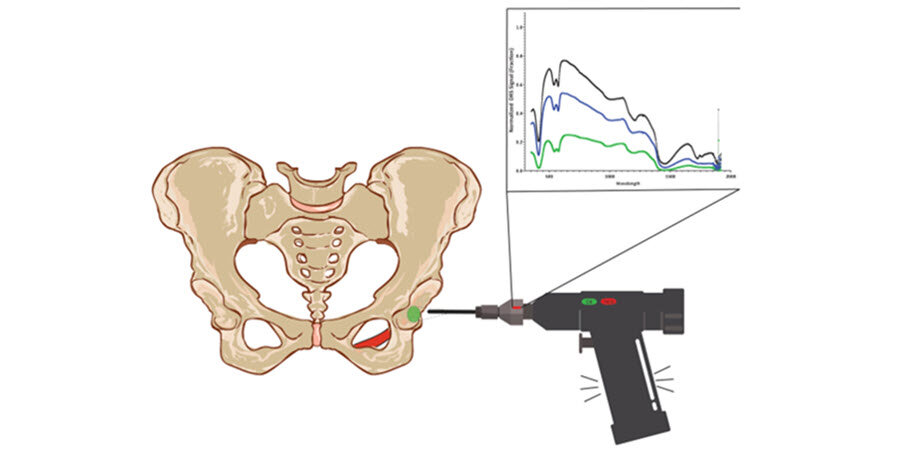
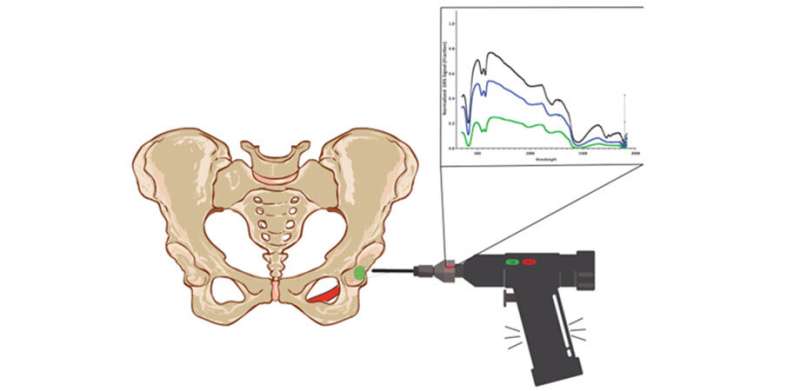
There are many types of optical sensing, and their use depends on the type of information required. For example, optical coherence tomography (OCT) enables imaging of tissue microstructures, whereas Raman spectroscopy can report the molecular signatures of tissue. Such techniques may be applied to help guide a surgical procedure, alone or in combination, at the working tip of a surgical instrument. For instance, by sensing the inherent optical properties of bone and its surrounding tissues, an optically equipped surgical drill would enable discernment of bone/tissue interfaces to increase surgical accuracy. Surgeons would benefit from visual cues provided by the optical sensor, such as a green light to indicate when a drill bit is in the correct bone zone, or a warning light when it approaches a boundary—say, collagen, blood, myelin, or lipids. Currently, auditory or sensory feedback provides that information.
What is needed for optical sensing in a drill bit? Routine hip surgery involves a drill bit with a flexible, hollow core, which is a convenient location for fiberoptics, but the glass fibers commonly used for optical sensing are not so flexible. Flexible fibers could be made of plastic, but how long would they last in such an environment? This is just one of many challenges that must be addressed to enable integration of optical sensing for delicate surgical instruments.
The team envisions multiple scenarios in which optical sensing would increase accuracy and improve outcomes. Reviewing recent developments in optics-enabled orthopedic technologies and unmet clinical needs for surgical instruments, the authors provide pragmatic guidance for innovation. Submillimeter accuracy is an optimal goal, necessary for spinal surgery.
According to lead author Carl Fisher, “any optical approach that could approximate CT guidance would be beneficial, as it would reduce requirements for CT and radiation exposure.” Identifying and incorporating tissue-specific optical properties for bone and soft tissues, as well as connective tissues and neurovascular tissues, is important groundwork.
Source: Read Full Article