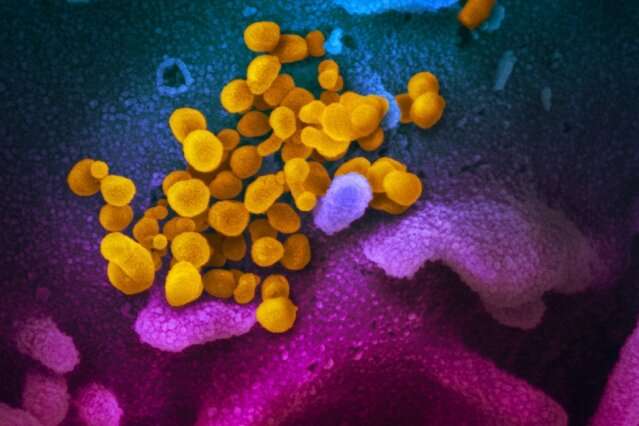
The differing immune system responses of patients with COVID-19 can help predict who will experience moderate and severe consequences of disease, according to a new study by Yale researchers published July 27 in the journal Nature.
The findings may help identify individuals at high risk of severe illness early in their hospitalization and suggest drugs to treat COVID-19.
Researchers examined 113 patients admitted to Yale New Haven Hospital, and analyzed the varying immune system responses they exhibited during their hospital stay, from admittance to discharge or death. They found that all patients shared a common COVID-19 “signature” in immune system activity early in the course of disease. But those who experienced only moderate symptoms exhibited diminishing immune system responses and viral load over time. Patients who went on to develop severe cases of the disease showed no decrease in viral load or immune system reaction, and many of the immune signals in these patients accelerated.
But even in the early course of treatment, researchers found indicators that predicted which patients were at greatest risk of developing severe forms of the illness.
“We were able to pull out signatures of disease risk,” said senior author Akiko Iwasaki, the Waldemar Von Zedtwitz Professor of Immunobiology and Molecular, Cellular and Developmental Biology and investigator for the Howard Hughes Medical Institute.
Researchers had known that the immune system unleashed a massive and damaging “cytokine storm” in severe cases of COVID-19. But the specific elements of the immune system response most responsible for the damage were unknown.
The Yale analysis found some intriguing links to poor outcomes. Curiously, said researchers, one risk factor was the presence of alpha interferon, a cytokine mobilized to combat viral pathogens such as the flu virus. However, COVID-19 patients with high levels of alpha interferon fared worse than those with low levels.
“This virus just doesn’t seem to care about alpha interferon,” Iwasaki said. “The cytokine appears to be hurting, not helping.”
Another early prognosticator of poor outcomes is activation of the inflammasome, a complex of proteins that detects pathogens and triggers an inflammatory response to infection. Inflammasome activation was linked to poor outcomes and death in several patients.
Researchers found that people who respond better to the infection tend to express high levels of growth factors, a type of cytokine that repairs tissue damage to the linings of blood vessels and lungs.
Taken together, the data can help predict patients at high risk of poor outcomes, the authors said.
Source: Read Full Article
