For the first time, an expert medical group has recommended delaying, decreasing and simplifying cervical cancer screening, largely because the HPV vaccine, introduced 14 years ago, is protecting young women from the disease.
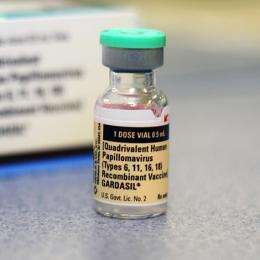
Most Americans still don’t know that the human papillomavirus, or HPV, causes oral and genital cancers, and too many parents are not getting their preteens vaccinated, studies show. But studies also show that even without optimal vaccination rates, Merck’s Gardasil shots have been a public health victory, dramatically reducing the precancerous cervical lesions that can progress to cancer, as well as the oral infections that have fueled an explosion in head and neck cancers in recent decades, particularly in men.
That’s why the American Cancer Society last month updated its cervical cancer guidelines: Women should start screening at age 25, not 21 as previously recommended. And they don’t need the hit-or-miss Pap smear, which checks a scraping of cervical cells under a microscope. Instead, cervical cells should be collected just once every five years and analyzed to see if they harbor HPV genetic material (DNA).
If the DNA test is positive, the patient may need more frequent follow-up visits, or a procedure to examine the cervix for signs of disease.
“These streamlined recommendations can improve compliance and reduce potential harms” of screening, said Debbie Saslow, an American Cancer Society expert on HPV and gynecological cancers. “They are made possible by some important developments that have allowed us to transform our approach to cervical cancer screening, primarily a deeper understanding of the role of HPV and the development of tools to address it.”
The American College of Obstetricians and Gynecologists said it will review the cancer society’s new advice “to determine whether a similar update to our guidance is needed.”
The goal of screening is to find ominous changes in cervical cells so they can be removed or destroyed before they become malignant. Over the last half-century, this strategy has crushed what was once the leading cancer killer of U.S. women. In 2020, about 13,800 women will be diagnosed with cervical cancer and 4,000 will die of it, the cancer society estimates.
Then again, treatment must be used judiciously because it can damage the cervix and complicate a later pregnancy.
Because of the evolving science and technology, cervical cancer screening guidelines have become more and more complicated over the past few decades. The 60-year-old Pap test remains important, and some doctors still default to annual screening with it. But the discovery in the 1980s that certain strains of HPV cause cancer led to the development of Gardasil, introduced in 2006, and the HPV DNA test.
Using DNA tests for screening has been controversial. While several brands have been approved for use as a “co-test” with the Pap smear, only two DNA tests have been deemed good enough to be used as a stand-alone, or “primary,” screening method—and not all labs offer them.
By 2018, expert groups, including an influential government advisory panel, recommended the same thing: a confusing menu of options for screening every three or five years, depending on the woman’s age and the choice of tests. Women in their 20s were advised to get a Pap smear every three years—even if they had been vaccinated. But they were not supposed to get DNA tests for fear that detecting the transient HPV infections that are common in this age group might lead to unnecessary monitoring and treatment.
The cancer society’s new guidelines say Pap smears or co-testing are still “acceptable options,” but primary HPV DNA testing is “preferred” because “data suggest vaccination has led to a drop in rates of precancerous cervical changes.”
Indeed, an international review published in 2016 found that in developed countries, the HPV vaccine had reduced cervical precancers by as much as 85%, and less severe cervical abnormalities by as much as 45%.
The cancer society estimated that less frequent screening using HPV DNA tests alone, starting at age 25, would prevent 13% more cervical cancers and 7% more deaths—with 45% fewer tests overall.
Of course, even simpler won’t be easy.
Source: Read Full Article
