“You just have bad cramps,” was the typical response teenager Sarah Swenson heard when she complained about the excruciating pain she experienced every time she had her period.
“It felt like someone was stabbing me with a hot poker,” says Sarah, 16, a resident of Madison and a high school junior.
Eventually, the pain became so severe she needed to use a wheelchair to get around in school. She had to stop playing her flute because it hurt to take a deep breath. An honors student active in marching band, robotics club, fencing, lyrical dance, and Girl Scouts, Sarah was a shell of herself from June to December of 2019.
Sarah’s parents—both of whom are physicians—were beside themselves. They took her to countless doctors. Appendicitis, gastrointestinal problems, and nerve disorders were all ruled out. A pain specialist even tried an abdominal nerve block. Nothing provided relief.
Meanwhile, during this time frame, Sarah ended up in the emergency department (ED) numerous times. “I was sobbing the entire time, knowing these weren’t just regular period cramps,” Sarah recalls of one car ride to the ED in June of that year.
At that hospital trip, doctors detected a cyst on Sarah’s right ovary. She was almost glad; finally, she thought she had an explanation. Sarah and her parents were told that an ovarian cyst is usually not dangerous in a girl her age unless it bleeds or twists the ovary, cutting off its blood supply. Over time, she was told, it would likely resolve on its own.
One diagnosis ruled out
Over the summer, however, the pain did not resolve. In September of that year, just after school started, the discomfort reached a new peak and Sarah was admitted to the hospital. To her surprise, the cyst had disappeared completely. This suggested that the ovarian cyst was not the problem. Blood tests, ultrasounds, CT scans, and MRIs all revealed nothing. She began experiencing severe pain in her right lower abdomen all the time, and when she had her period it was dramatically worse. Sarah was missing many school days and struggling to keep up in her classes.
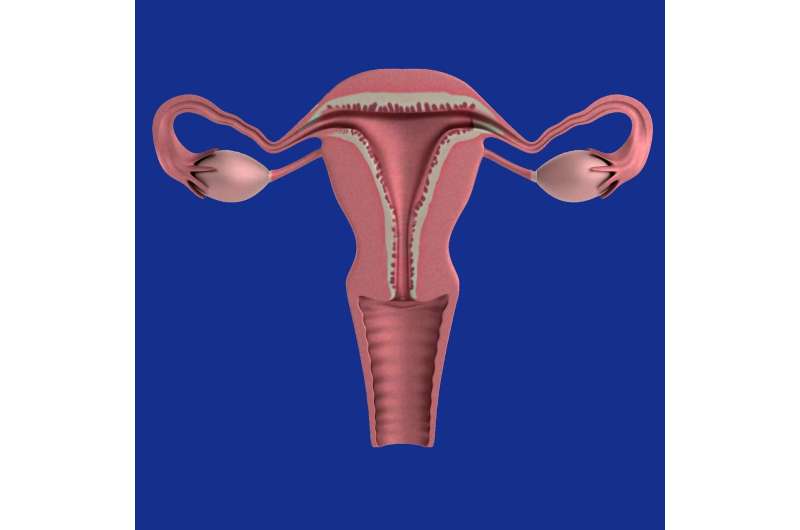
Early on, Sarah’s mother, Jennifer Swenson, had wondered if her daughter might have endometriosis, a condition in which tissue similar to the lining of the uterus (endometrium) grows outside of it, often on the ovaries and fallopian tubes. The tissue swells and bleeds during a woman’s menstrual period, leading to pain, and sometimes inflammation and scar tissue.
Medical experts don’t know for sure what causes endometriosis, but there are many possibilities, including retrograde menstrual flow (when endometrial tissue shed during a woman’s period inadvertently goes through the fallopian tube into other parts of the body), genetic factors, and hormone problems.
The Swensons consulted multiple obstetrician-gynecologists about the possibility that Sarah might have endometriosis, but were told she was “definitely too young.” The condition is most common in women in their 30s and 40s.
An answer at last
Still, her mother persisted and booked an appointment for her daughter with Alla Vash-Margita, MD, a Yale Medicine pediatric and adolescent gynecologist. “Dr. Vash-Margita listened to our story and said, “I think this is endometriosis. We just have to prove it,'” Jennifer recalls.
The only way to diagnose endometriosis is to perform laparoscopic surgery (minimally invasive surgery with a small incision) and obtain a biopsy. The surgery was scheduled for a few weeks later and, in the meantime, Dr. Vash-Margita started Sarah on a progestin pill. Progestin—a synthetic form of the hormone progesterone—suppresses progression of the growth of the endometrial tissue outside the uterus.
“During the first phase of the menstrual cycle, estrogen makes the endometrium grow, and then in the second phase, the ovaries produce progesterone, which makes the tissue shed,” Dr. Vash-Margita explains. “But if that shedding happens outside the uterus, you will feel pain in all of those other places where it sheds. There is a theory that endometriosis is fueled by estrogen. So, if you stop the endometrium from growing with a progestin pill, it can keep the problem at bay.”
When endometrial-like tissue grows outside of the uterus, it forms endometriotic lesions. These lesions irritate the lining of the abdominal cavity, causing pain. Endometriosis can also lead to adhesions, or scar tissue that forms between organs in the pelvis and abdomen. If endometriosis goes undetected, over time adhesions can cause damage to affected organs and, even, infertility.
During Sarah’s surgery in late October of 2019, Dr. Vash-Margita visualized (and took biopsies of) endometriotic lesions, and she took out those that could be safely removed. The biopsy results confirmed a diagnosis of Stage III endometriosis, a moderate form of the disease, Dr. Vash-Margita says. The first line of treatment is hormonal therapy, which is what she’d already started for Sarah.
When Dr. Vash-Margita came out of the operating room and shared the news with Sarah’s parents, Jennifer began to cry. “We were so relieved,” she says. “We finally had an answer and could start treating it.”
Dr. Vash-Margita increased the dose of Sarah’s progestin pill.
A return to normalcy
After the surgery, Sarah was still weak, but she insisted on going to school within a few days. “It was Halloween, and I had a really cool costume. I was Scooby-Doo and had turned my wheelchair into the Mystery Machine,” says Sarah.
Slowly, she returned to her activities, including playing the flute and fencing. Because the progestin medication suppresses her menstrual cycle, Sarah no longer gets her period, and she is pain-free. “It took several months after starting progestin for her to feel back to normal,” says Jennifer.
Sarah will stay on the progestin pill and check in with Dr. Vash-Margita a few times a year. Because the medication stops the natural production of estrogen, which protects against bone loss, Sarah has been advised to do weight-bearing exercises and to take calcium and vitamin D supplements.
While the Swensons are grateful that Sarah is now in good health, they are still reeling from the traumatic experience.
“The most frustrating thing was the lack of awareness that someone her age could have endometriosis. There was a bias that it just doesn’t happen, that she was too young,” says Sarah’s father, Scott Swenson.
Indeed, there is a common misconception that endometriosis does not occur in girls or young women, Dr. Vash-Margita says. “There are published studies about endometriosis in adolescents, and I have a cohort of biopsy-proven cases of my own,” she says. “This is a shame, as these teens miss school and activities, and late diagnosis leads to other health problems.”
For adult women, it takes two to four years to reach a diagnosis of endometriosis, but for teens it is six to 10 years, on average, after symptoms begin.
“The pain in adolescents is not always as cyclical as it is in adult women, meaning it’s not necessarily tied to their period,” she explains. “It may be present throughout the entire menstrual cycle, which throws doctors off. As a faculty member at Yale University, I teach medical students and residents to make sure they are aware of this diagnosis as one of the causes of pelvic or abdominal pain in young girls. I also want girls to know they shouldn’t live with pain when they have their periods. We can investigate and help.”
Another reason endometriosis can be difficult to diagnose is that the tests require a surgical procedure. However, Yale researchers, including Dr. Vash-Margita, are investigating blood and saliva tests that could detect it in a noninvasive way.
As for Sarah, the experience taught her a valuable lesson about how to advocate for oneself when it comes to medical problems. “You have to stick up for yourself. If something is wrong, insist on finding an answer,” she says. “You know your body best, and don’t let someone dismiss you and say nothing is wrong just because you don’t see it.”
Even with their medical backgrounds, Sarah’s parents say they had to fight for answers.
“She was lucky she had a mom who is a physician. I kept pressing for answers, and we had a diagnosis within six weeks of her being in the hospital the last time,” Jennifer says. “Most cases would take years.”
Meanwhile, Sarah plans to frame her Girl Scouts Gold Award—a service project and the highest award in the organization—around endometriosis awareness as a way to help other girls avoid what she went through.
She’s thinking the project may entail creating educational pamphlets for school nurses and pediatricians to have handy when girls visit them with menstrual complaints. Already, she says her research has shown there is little information out there about endometriosis in young girls.
Source: Read Full Article
