Dental root voids are commonly obturated with polymer materials that harden after injection. Research is exploring the use of hydrogels seeded with pluripotent stem cells to regenerate the natural tooth material from the inside of the filling, instead of gluing the voids with hardening polymers.
Scientists have now shown that a composite material of titanium oxide and polyisoprene (PI), the major component of the approved root void filling material Gutta-percha, can induce the differentiation of dental stem cells and activate the biomineralization of dental-like material.
Skip to:
- Controlling the Hardness of Polymer-mineral Composites
- Cells Adapt to the Hardness of Their Surrounding
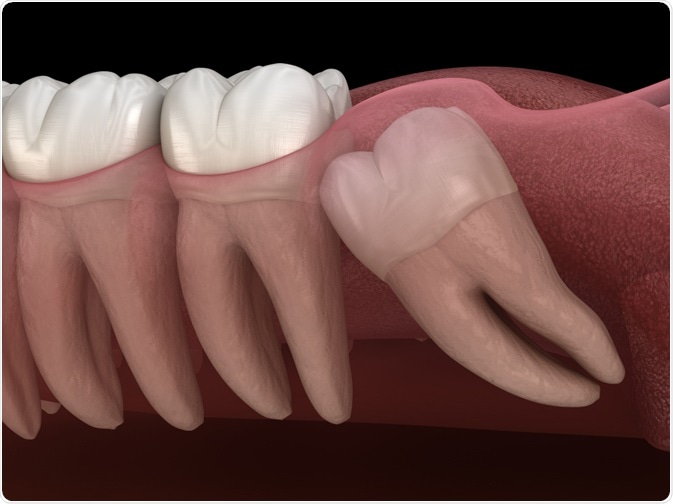 Image Credit: Alex Mit / Shutterstock.com
Image Credit: Alex Mit / Shutterstock.com
This research is published in the April edition of the journal Acta Biomaterialia.
Many fractures of hard tissues (i.e. bone or dental material) can regenerate and the fractures become closed. However, if a fracture creates a large void, the regeneration becomes challenging as for instance, two pieces of bone need to grow towards each other across a gap.
To facilitate the regeneration, attempts have been made to fill such voids with hydrogels that accommodate pluripotent stem cells (PSCs). These PSCs can subsequently be differentiated into biomineralizing cell types that form calcium phosphates, the major component of both teeth and bone.
The hydrogels serve as an artificial extracellular matrix to which the PSCs can adhere so that the biomineralization activity is spread throughout the gel.
In vitro, the differentiation of PSCs can be induced by chemicals such as dexamethasone. However, when using such mobile, diffusible chemicals it needs to be ensured that these do not cause effects on adjacent tissues. As an alternative, several lines of evidence suggest that the mechanic features, i.e. stiffness of hydrogels can serve as an inducer of cell differentiation.
Researchers from the USA and China, led by Professors Miriam Rafailovich and Liudi Zhang, have now shown in vitro that titanium oxide-enforced thin films of the polymer polyisoprene (PI), the major component of Gutta-percha, activate the biomineralization of calcium phosphate from seeded dental pulp stem cells (DPSC).
Controlling the Hardness of Polymer-mineral Composites
The scientists used spin coating to deposit polymer layers of 15 to 210 nm, with and without titanium oxide enforcement, on a plane silicon wafer. They seeded DPSCs onto these layers and assessed their growth by microscopic techniques.
The scientists demonstrated the activation of biomineralization pathways by quantitative PCR, targeting genes that are commonly up-regulated upon differentiation of stem cells into biomineralizing cells. Finally, the biomineralization was directly confirmed by electron microscopy with elemental analysis of mineral deposits by electron dispersive X-ray analysis (EDS).
To understand how the cells respond to the hardness of the polymer-mineral composite, the scientists additionally measured the stiffness of the cell membrane and the cellular interior. For this measurement, they used an optical tweezer-based rheology technique where an oscillating laser sets a micrometer-sized silica particle in motion, and the movement-response of the particle at constant laser energy allows to determine the stiffness of the particle’s surrounding.
Silica particles were taken up by cells spontaneously or were directed to the membrane by a specific antibody coating.
Cells Adapt to the Hardness of Their Surrounding
The scientists observed that the cells activated biomineralization pathways and deposited calcium phosphates when growing on 15 nm PI thin films. The 210 nm PI films alone did not induce biomineralization, however, calcium phosphate deposits were found when these thicker films had been hardened by the addition of titanium oxides.
The investigators concluded that it is indeed the film's hardness that can induce the biomineralization activity. They found that the cell interior adapted to the hardened surrounding by developing a stronger cytoskeleton, which in turn stiffened the cells in rheology measurements.
This research gives support to the idea of using polymer and polymer-mineral composites as a scaffold for PSC culture implants as a potential avenue for regenerative medicine. Making use of the mechanics of the materials to induce PSC differentiation could avoid chemical differentiation factor additives that can be lost from the gel by diffusion and cause an effect in surrounding tissue.
To envision a medical use, the hardness-controlled composite materials would need to be biocompatible and non-toxic, and the scientists took this into account by using the polymer polyisoprene (PI) which is already approved for dental filling materials, and inert titanium oxide minerals.
However, while the researchers studied the cell cultures on PI thin films, PI-based dental fillers need to be dissolved in organic solvents to inject them into a void, and cells would not survive exposure to commonly used solvents.
Future work towards injectable PSC-gels can now build on the findings that a mineral-hardened polyisoprene matrix can be used to differentiate DPSCs, by testing other hardness-controlled composite formulations that also might allow PSC-seeding before injection.
Source
Chuang YC et al., Regulating substrate mechanics to achieve odontogenic differentiation for dental pulp stem cells on TiO2 filled and unfilled polyisoprene. Acta Biomaterialia 2019, 89, 60-72; DOI: 10.1016/j.actbio.2019.02.040.
Further Reading
- All Stem Cells Content
- Stem Cell Sources, Types, and Uses in Research
- What are Stem Cell Transplants?
- Stem Cell Properties
- What are Stromal Cells?
Last Updated: Nov 5, 2019

Written by
Christian Zerfaß, Ph.D.
Christian is an enthusiastic life scientist who wants to understand the world around us. He was awarded a Ph.D. in Protein Biochemistry from Johannes Gutenberg University in Mainz, Germany, in 2015, after which he moved to Warwick University in the UK to become a post-doctoral researcher in Synthetic Biology.
Source: Read Full Article
