
“Can you draw me a picture of your headache?” may sound like an unusual question—but drawings of headache pain provide plastic surgeons with valuable information on which patients are more or less likely to benefit from surgery to alleviate migraine headaches.
Patients with more “typical” patterns on pain sketches have larger reductions in headache scores after migraine “trigger site” surgery, suggests a new study by Lisa Gfrerer, MD Ph.D. and William Gerald Austen, Jr., MD, and colleagues of Harvard Medical School. The study appears in the October issue of Plastic and Reconstructive Surgery, the official medical journal of the American Society of Plastic Surgeons (ASPS).
Migraine surgery has become an established treatment alternative for some patients with intractable migraine headaches. Developed by plastic surgeons who noticed that some migraine patients had fewer headaches after cosmetic forehead-lift, migraine surgery targets specific trigger sites linked to certain headache patterns. More than 5,200 patients underwent migraine peripheral trigger site surgery in 2019, according to ASPS statistics.
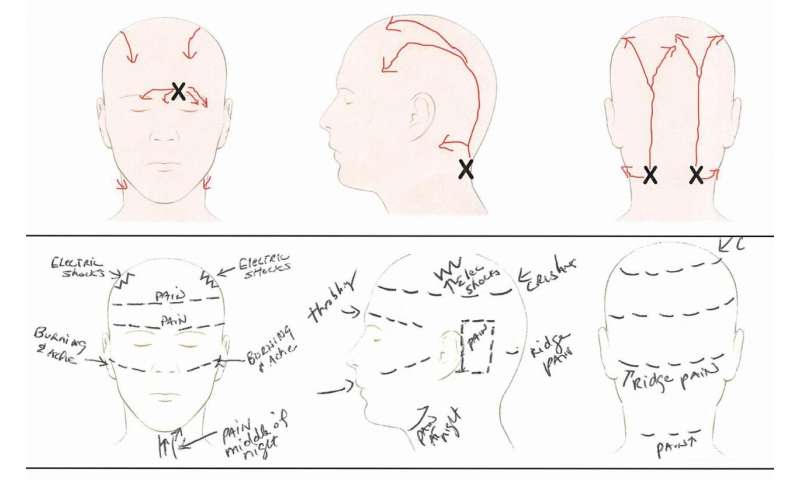
However, it can be difficult to predict which patients will get good results from migraine surgery. Drs. Gfrerer, Austen and colleagues have noticed that there are “pathognomic” pain patterns for each trigger site. “In our experience, a valuable method to visualize pain/trigger sites is to ask patients to draw their pain,” the researchers write. In the new study, they analyzed how well the patterns on these pain drawings predict the outcomes of migraine surgery.
The study included 106 patients who made pain sketches as part of their evaluation for migraine surgery. The sketches were reviewed by experienced researchers who were unaware of the patients’ headache symptoms or other characteristics, and classified into three groups:
- Typical – showing pain originating from and spreading along the expected path of a specific nerve (59 percent of sketches)
- Intermediate – showing pain along the path of the nerve, but with an atypical spread (radiation) of pain (29 percent)
- Atypical – pain originating and radiating outside of the expected nerve distribution (12 percent)
One year after surgery, outcomes were assessed using a standard score, the Migraine Headache Index (MHI). Patients with typical or intermediate patterns on their pain drawings had similarly good outcomes: MHI scores improved by 73 and 78 percent, respectively.
However, for patients with atypical pain sketches the results were not as good: only 30 percent improvement in MHI score. Just one-fifth of patients in the atypical group had more than 30 percent improvement after migraine surgery.
The researchers emphasize that pain drawings should be just one part of the standard patient assessment. Migraine patients with atypical pain drawings may still have “compelling reasons” for surgery but should understand that they have lower chances of a positive outcome.
Source: Read Full Article
